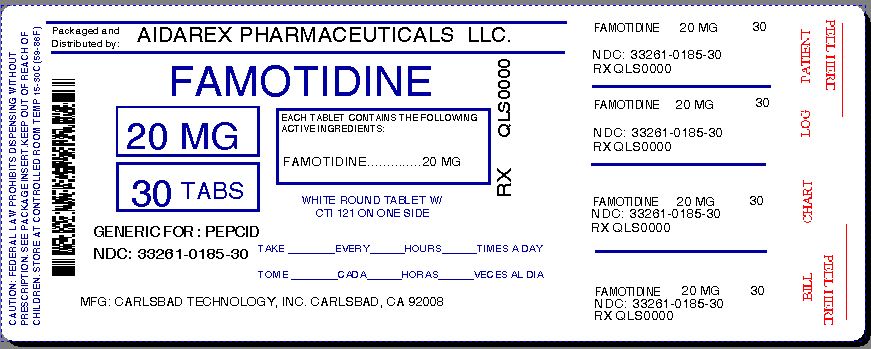
Famotidine Tablet while Breastfeeding
What is Famotidine Tablet used for?
Is Famotidine Tablet usage safe while breastfeeding? If a lactating mother is using it can there be any effect on growth or development of infant?

Nursing Mothers Studies performed in lactating rats have shown that famotidine is secreted into breast milk. Transient growth depression was observed in young rats suckling from mothers treated with maternotoxic doses of at least 600 times the usual human dose. Famotidine is detectable in human milk. Because of the potential for serious adverse reactions in nursing infants from famotidine, a decision should be made whether to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.
Famotidine Tablet Breastfeeding Analsys
Famotidine while Breastfeeding
SafeCAS Number: 76824-35-6
H2-type histamine receptor antagonist with similar action than cimetidine. It is excreted in breast milk in clinically non-significant amount, much less than the dose administered to newborns and infants with gastroesophageal reflux disorders. Although it does not normally affect prolactin secretion, there have been several cases of galactorrhea. Still unknown whether it is due to Famotidine itself or to gastroesophageal reflux. Famotidine, Nizatidine and Roxatidine are excreted into milk but in less proportion than Cimetidine or Ranitidine, which have been proposed as alternative to during lactation.
Famotidine Tablet Breastfeeding Analsys - 2
Famotidine while Breastfeeding
CAS Number: 76824-35-6
Famotidine is used in newborn infants in higher dosages than are transmitted in breastmilk.[1] Famotidine would not be expected to cause any adverse effects in breastfed infants. No special precautions are required.
What if I already have used Famotidine Tablet?
As usage of Famotidine Tablet is mostly safe while breastfeeding hence there should not be any concern. In case of any change in behavior or health of your baby you should inform your health care provider about usage of Famotidine Tablet else no further action is required.
I am nursing mother and my doctor has suggested me to use Famotidine Tablet, is it safe?
Definitely, Famotidine Tablet is safe in lactation for baby. No wonder your doctor has recommended it.
If I am using Famotidine Tablet, will my baby need extra monitoring?
No extra baby monitoring required while mother is using Famotidine Tablet
Who can I talk to if I have questions about usage of Famotidine Tablet in breastfeeding?
US
National Womens Health and Breastfeeding Helpline: 800-994-9662 (TDD 888-220-5446) 9 a.m. and 6 p.m. ET, Monday through Friday
UK
National Breastfeeding Helpline: 0300-100-0212 9.30am to 9.30pm, daily
Association of Breastfeeding Mothers: 0300-330-5453
La Leche League: 0345-120-2918
The Breastfeeding Network supporter line in Bengali and Sylheti: 0300-456-2421
National Childbirth Trust (NCT): 0300-330-0700
Australia
National Breastfeeding Helpline: 1800-686-268 24 hours a day, 7 days a week
Canada
Telehealth Ontario for breastfeeding: 1-866-797-0000 24 hours a day, 7 days a week
