Oligo Bio Iodine 60 Ml while Breastfeeding
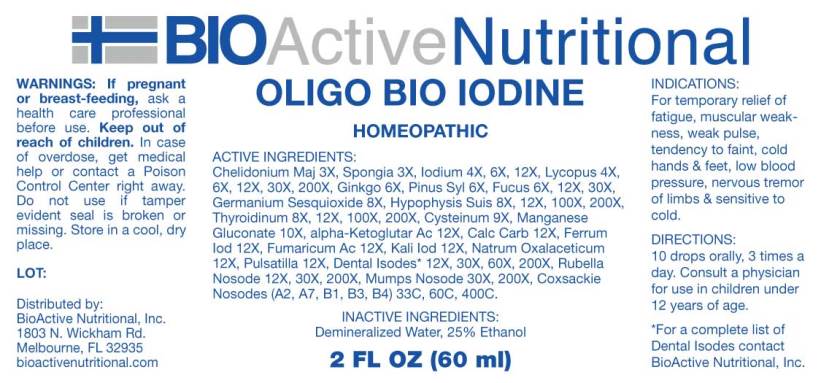
What is Oligo Bio Iodine 60 Ml used for?
Is Oligo Bio Iodine 60 Ml usage safe while breastfeeding? If a lactating mother is using it can there be any effect on growth or development of infant?

Oligo Bio Iodine 60 Ml Breastfeeding Analsys
Iodine while Breastfeeding
UnsafeCAS Number: 7553-56-2
Disinfectant that contains high amount (2-7%) of Iodine in solution with alcohol or water (Lugol's solution) Not absorbed through intact skin of adults. However, it may trespass the inflamed skin, wounds, mucosa surfaces like vagina, in which case can reach concentration in grams in the human serum (1 g = 1,000 milligrams = 1,000,000 micrograms). Normal daily allowance is considered to be as high as 100 to 150 micrograms that increases to 200 – 300 micrograms in pregnancy or nursing period. The latter means less than one third of a milligram. Iodine is concentrated into breast milk with a level that could reach 20 times higher than the concentration in the blood. It has been found higher levels of Iodine, altered results of neonatal screening test for thyroid function, and, transient hypothyroidism in infants whose mothers were exposed to Iodine Povidone. Use should be avoid in the Delivery Room, Operating Room (C-section), Neonatal Units, Toddler admision areas and during the breastfeeding period. Sporadic or inadvertent use, specially on normal skin, does not require special test or procedures because it does not pose higher risk to the child.
Ginkgo while Breastfeeding
Low RiskCAS Number: 90045-36-6
Leaves of tree are used.It contains flavonoids, tannins, diterpenes, steroids..Unproved effects: venous tonic, capillary protector, vasodilator (neuron-protector) and platelet anti-aggregationIndications after Commission E of German Ministry of Health: brain vascular insufficiency, intermittent claudication, dizziness, tinnitus. Fluids or solutions with alcoholic content are to be avoided.
Pinus sylvestris leafy twig while Breastfeeding
UnsafeGems, leaves, tender branches and bark are used. Leaves and gems contain trementine, essential oil and colophony. Bark contains flavonoids, anthocyanides, trementine and tannins. Commission E of German Ministry of Health has approved the use of essential oil and trementine for treatment of common cold and topical use on joints, muscles and neural pain. Trementine use is contraindicated while pregnancy, suckling and childhood. Bark extractor (Pycnogenol) which is traditionally used as blood vessel protector and anti-oxidative agent is not contraindicated during breastfeeding.
Fucus vesiculosus while Breastfeeding
UnsafeSeaweed. The stem of the plant is used.It contains large amounts of mucilage and minerals, including iodine which appears in variable amounts that can be significant, in such a way that it may be a cause a hyperthyroidism-like disease (anxiety, insomnia, tachycardia, palpitations).It may also contain heavy metals, being a species of seaweed with a high ability of contamination by toxic products. The commission E of the German Health Ministry has not approved any clinical indication, discouraging its use. At latest update no published data on excretion into breast milk were found. However, there is information from other algae whose consumption is known to increase iodine levels in the plasma and breast milk.There have been reports of hypothyroidism in infants whose mothers have included in their diet important quantities of seaweed. There is no evidence of effectiveness on increasing milk production. The most effective method to increase milk production should be done by strengthening maternal self-confidence, evaluate and correct problems along with an effective support to breastfeeding mothers.
Oyster shell calcium carbonate, crude while Breastfeeding
SafeCAS Number: 471-34-1
Various calcium salts (Acetate, Carbonate, Chloride, Citrate, Phosphate, Gluceptate, Glucobionato, Lactate, Laxctobionato Pidolate, Silicate) are used in the management of hypocalcemia, supplements for treating calcium deficiency states and antacids ( Carbonate and Silicate) Daily requirement of calcium during lactation are 1 g (1.3 g in children under 20 years).Calcium supplements in the diet does not affect the concentration of calcium in milk.Excessive intake of calcium is not good for health. During lactation, consumption of calcium should not exceed 2.5 g a day. WHO List of Essential Medicines 2002 states that it is compatible with breastfeeding.
Fumaric acid while Breastfeeding
Low RiskCAS Number: 110-17-8
Anti-inflammatory and immunomodulator used in the treatment of psoriasis and in relapsing forms of multiple sclerosis. Since the last update we have not found published data on its excretion in breast milk. Its pharmacokinetic data (large volume of distribution and short half-life) make it unlikely that milk would pass through in significant quantities (Almas 2016).Possible side effects are rare and generally not serious, with no immunosuppressive effects or higher frequency of infections (EMA 2017, AEMPS 2015). Until there is more published data on this drug in relation to breastfeeding, known safer alternatives may be preferable, especially during the neonatal period and in case of prematurity (Brown 2017, Yiu 2015, Bove 2014, Cree 2013).
Iodide ion while Breastfeeding
UnsafeCAS Number: 7553-56-2
Disinfectant that contains high amount (2-7%) of Iodine in solution with alcohol or water (Lugol's solution) Not absorbed through intact skin of adults. However, it may trespass the inflamed skin, wounds, mucosa surfaces like vagina, in which case can reach concentration in grams in the human serum (1 g = 1,000 milligrams = 1,000,000 micrograms). Normal daily allowance is considered to be as high as 100 to 150 micrograms that increases to 200 – 300 micrograms in pregnancy or nursing period. The latter means less than one third of a milligram. Iodine is concentrated into breast milk with a level that could reach 20 times higher than the concentration in the blood. It has been found higher levels of Iodine, altered results of neonatal screening test for thyroid function, and, transient hypothyroidism in infants whose mothers were exposed to Iodine Povidone. Use should be avoid in the Delivery Room, Operating Room (C-section), Neonatal Units, Toddler admision areas and during the breastfeeding period. Sporadic or inadvertent use, specially on normal skin, does not require special test or procedures because it does not pose higher risk to the child.
Silver while Breastfeeding
SafeCAS Number: 7761-88-8
Avoid using it on the breast or cleanse thoroughly before nursing.
Gold while Breastfeeding
Low RiskCAS Number: 7440-57-5
One case of facial edema that was barely related to this drug has been described. It has an extremely long half-life span.
Formaldehyde while Breastfeeding
UnsafeCAS Number: 50-00-0
It is a highly volatile gas that is irritating to respiratory, ocular and cutaneous tissues. The olfactory threshold is so low that poisoning can easily be prevented. Used for many industrial procedures (wood, cosmetics, paint, plastics, resins, chemistry, textiles, photography) and in the preservation of corpses and histological specimens. A largest source of exposure is the combustion process (ATSDR 1999 and 2008) Formaldehyde is a known carcinogen factor especially on the nasopharyngeal tract (NCI 2011, INSHT 2015, USDHHS 2016). Although mild hormonal changes have been seen in women exposed to organic solvent mixtures with formaldehyde (Hassani 2014), few data is available in the scientific literature on the transfer of chemicals to breastmilk from working mothers (Giroux 1992, Fisher 1997). Despite the growing concern about labor exposure of formaldehyde in lactating mothers (Grajewski 2016), data sheets consulted on formaldehyde (LabKem 2013) do not offer any statement on risk or warning advice in connection to breastfeeding (LabKem 2013) (Phrases R 33, R 64, H 362 and P 263). It undergoes a rapid destruction in the plasma and tissues, so it is believed that formaldehyde whether inhaled or in contact with the skin would highly unlikely any transfer from the mother to the infant through the breastmilk (ATSDR 1999). However it may occur in work places with high levels of exposure such as pathology departments and forensic facilities (CDC-NIOSH 2015, Appendix A 2016). Because of this, several agencies recommend as a prudent measure for breastfeeding women to be removed from duties that involve high exposure levels of formaldehyde (Appendix A 2016). If the company does not agree with the exchange of the working site of a highly exposed lactating mother, they should ensure adequate working conditions of protection (CDC-NIOSH 2015: masks, gloves) and well ventilated facilities that must be able to keep VLA-EC ( TLV-STEL) below 0.3 ppm (0.37 mg / m 3) (USDHHS 2016). Avoid to breastfeeding if the mother has been massively intoxicated by inhalation or ingestion. The benefits of breastfeeding outweigh the risk posed by low levels of environmental contaminants contained in human milk, which are often lower than those contained in cow's milk or other foods (WHO).
Lidocaine while Breastfeeding
SafeCAS Number: 137-58-6
Compatible with breastfeeding no matter the multiple ways it can be used: anesthetic, anti-arrhythmic, or anti-epileptic drug. Excreted into breast milk in non-significant amount with no side effects on breastfed infants from treated mothers. As a topical anesthetic (dermatologic, dental-stomatologic, ophtalmotologic and otologic preparations) it has an almost nil systemic absorption. Avoid using it on the nipple, but if necessary do it after the breast feed, wipe it out and rinse with water before the next feed, An euptectic mixture with added Prilocaine (EMLA) is used for dermatologic anesthesia. There is an increased risk of Methemoglobinemia when applied on large surfaces or taken by mouth. Intrapartum anesthesia may delay the onset of phase II of Lactogenesis or milk coming-in. The American Academy of Pediatrics rates it usually compatible with Breastfeeding.
Mercurius solubilis while Breastfeeding
Low RiskCAS Number: 7439-97-6
Environmental pollutant that is used for manufacturation of batteries, fungicidal products, dental amalgam, and contaminated fish. Most of mercury present in breast milk does it as an inorganic substance which is almost non-absorbable. Breastfeeding should be discontinued whenever a mother is contaminated or intoxicated. It may be a source of neurological troubles. Benefits of breastfeeding are largely more important than risk related to the presence of mild level environment pollutants in human milk, in many instances, they are at lower content than those found in cow’s milk or other foods. (Codex alimentarius FAO-WHO).
Zinc while Breastfeeding
SafeZinc (Zn) is an essential element for nutrition. It is present in many foods.Recommended daily allowance of Zn is 8 to 15 mg. (Moran Hall 2010). Millions of people worldwide are Zn-deficient.It is used as a treatment for Wilson's disease and Acrodermatitis Enteropathica. Zn is involved in the regulation process of lactation (Lee 2016).Pasteurization of the milk does not affect the concentration of Zn and other trace elements (Mohd Taufek-2016). The average concentration of Zn in breastmilk is 4 to 16 mg / L (Picciano 1976, Hannan 2005, Dórea 2012) which is independent of plasma levels and maternal daily intake (Krebs 1995, Chierici 1999, Hannan 2009).Intestinal absorption of zinc is almost doubled during pregnancy and lactation (Fung 1997).Zinc levels in the infant are dependent on Zinc levels in the breast milk (Dumrongwongsiri 2015)With a varied and balanced diet, an extra intake of minerals is not needed. Excessive intake of Zinc may cause gastrointestinal problems and Pancytopenia (Irving 2003).
Rubella virus while Breastfeeding
SafeVaccine is made from live attenuated virus that may be excreted into breast milk. It is not a cause of serious harmful effects; one child reportedly has presented a type of mild Rubella after mother immunization. Vaccines are usually compatible with breastfeeding either if they are formed by live, attenuated, inactivated, death strains or microorganism toxoid. They are not excreted into breast milk and do not cause harm to the infant, except for rubella vaccine, but the virus usually does not infect the infant or if infection does occur, it is well tolerated because the virus is attenuated. Yellow fever vaccine has a higher risk for harm effect on infants younger than 6 months old (Consult information on a particular vaccine at our web). Breastfeeding may enhance antibody response to vaccines and cause fewer side effects as fever or anorexia. Early postpartum period is appropriate to get mothers vaccinated against measles, rubella, mumps and chicken-pox in case they were not immunized. Immunization of mothers with null or low Rubella-antibody levels at early postpartum is recommended. Breastfeeding mothers should be protected by providing recommended vaccination for adults.
Mumps virus while Breastfeeding
SafeLive attenuated virus vaccine. Vaccines are usually compatible with breastfeeding either if they are formed by live, attenuated, inactivated, death strains or microorganism toxoid. They are not excreted into breast milk and do not cause harm to the infant, except for rubella vaccine, but the virus usually does not infect the infant or if infection does occur, it is well tolerated because the virus is attenuated. Yellow fever vaccine has a higher risk for harm effect on infants younger than 6 months old (Consult information on a particular vaccine at our web). Breastfeeding may enhance antibody response to vaccines and cause fewer side effects as fever or anorexia. Early postpartum period is appropriate to get mothers vaccinated against measles, rubella, mumps and varicella in case they were not immunized. Breastfeeding mothers should be protected by providing recommended vaccination for adults.
Human coxsackievirus a2 while Breastfeeding
SafeVaccines are usually compatible with breastfeeding either if they are formed by live, attenuated, inactivated, death strains or microorganism toxoid. Except for rubella vaccine, they are not excreted into breast milk and do not cause harm to the infant. Yellow fever vaccine has a higher risk for harm effect on infants younger than 6 months old (Consult information on a particular vaccine at our web). Breastfeeding may enhance antibody response to vaccines. Early postpartum period is appropriate to get mothers vaccinated against measles, rubella and mumps in case they were not immunized. Breastfeeding mothers should be protected by providing recommended vaccination for adults.
Human coxsackievirus a7 while Breastfeeding
SafeVaccines are usually compatible with breastfeeding either if they are formed by live, attenuated, inactivated, death strains or microorganism toxoid. Except for rubella vaccine, they are not excreted into breast milk and do not cause harm to the infant. Yellow fever vaccine has a higher risk for harm effect on infants younger than 6 months old (Consult information on a particular vaccine at our web). Breastfeeding may enhance antibody response to vaccines. Early postpartum period is appropriate to get mothers vaccinated against measles, rubella and mumps in case they were not immunized. Breastfeeding mothers should be protected by providing recommended vaccination for adults.
Human coxsackievirus b1 while Breastfeeding
SafeVaccines are usually compatible with breastfeeding either if they are formed by live, attenuated, inactivated, death strains or microorganism toxoid. Except for rubella vaccine, they are not excreted into breast milk and do not cause harm to the infant. Yellow fever vaccine has a higher risk for harm effect on infants younger than 6 months old (Consult information on a particular vaccine at our web). Breastfeeding may enhance antibody response to vaccines. Early postpartum period is appropriate to get mothers vaccinated against measles, rubella and mumps in case they were not immunized. Breastfeeding mothers should be protected by providing recommended vaccination for adults.
Human coxsackievirus b3 while Breastfeeding
SafeVaccines are usually compatible with breastfeeding either if they are formed by live, attenuated, inactivated, death strains or microorganism toxoid. Except for rubella vaccine, they are not excreted into breast milk and do not cause harm to the infant. Yellow fever vaccine has a higher risk for harm effect on infants younger than 6 months old (Consult information on a particular vaccine at our web). Breastfeeding may enhance antibody response to vaccines. Early postpartum period is appropriate to get mothers vaccinated against measles, rubella and mumps in case they were not immunized. Breastfeeding mothers should be protected by providing recommended vaccination for adults.
Human coxsackievirus b4 while Breastfeeding
SafeVaccines are usually compatible with breastfeeding either if they are formed by live, attenuated, inactivated, death strains or microorganism toxoid. Except for rubella vaccine, they are not excreted into breast milk and do not cause harm to the infant. Yellow fever vaccine has a higher risk for harm effect on infants younger than 6 months old (Consult information on a particular vaccine at our web). Breastfeeding may enhance antibody response to vaccines. Early postpartum period is appropriate to get mothers vaccinated against measles, rubella and mumps in case they were not immunized. Breastfeeding mothers should be protected by providing recommended vaccination for adults.
Oligo Bio Iodine 60 Ml Breastfeeding Analsys - 2
Iodine while Breastfeeding
CAS Number: 7553-56-2
Iodine is an essential trace nutrient for all infants that a normal component of breastmilk. Infant requirements are estimated to be 15 mcg/kg daily in fullterm infants and 30 mcg/kg daily in premature infants.[1] Systematic reviews and studies on iodine nutrition found that iodine in breastmilk is adequate in iodine-sufficient countries, but in countries with iodine fortification of foods, many mothers did not obtain adequate iodine and that additional supplementation was desirable.[2][3][4][5] In iodine-deficient areas, supplementation of breastfeeding mothers with iodine appears to be more effective than direct supplementation of the infant in reducing infant iodine deficiency.[6] The American Thyroid Association recommends that breastfeeding women should supplement their diet with a daily oral supplement that contains 150 mcg of iodine, but sustained iodine intake while breastfeeding that exceeds 500 to 1100 mcg daily should be avoided.[7] A survey in the United States between 2011 and 2014 found that only 19% of lactating women used a dietary supplement that contained iodine.[8] The use of excessive amounts of iodine in the mother near term and during breastfeeding (e.g., seaweed soup) can increase breastmilk iodine levels and cause transient hypothyroidism in breastfed infants. The absorption of iodine can be marked after application to open wounds or mucous membranes. Exposure of mothers to unnecessary iodine who are or will be breastfeeding should be avoided or minimized to the extent possible by avoiding its use on maternal mucous membranes (e.g., vaginal use, wound therapy), avoiding prolonged contact time, avoiding repeated applications, and applying it to the smallest possible surface areas of the body. It is possible that maternal exposure to iodine near term could interfere with thyroid studies done as a part of newborn screening tests.
Ginkgo while Breastfeeding
CAS Number: 90045-36-6
Ginkgo (Ginkgo biloba) leaf contains flavonoids (e.g., quercetin, kaempferol, isorhamnetine) and several terpene trilactones (e.g., ginkgolides, bilobalide) as well as numerous minor components. Standardization is based on ginkgo flavone glycoside and terpenoid content. Raw ginkgo seeds contain potentially toxic cyanogenic glycosides and should not be used; roasted seeds do not carry this risk. Ginkgo has no specific uses during breastfeeding, but is commonly used as an antioxidant, a vasodilator to increase cerebral and peripheral perfusion, and to improve memory. No data exist on the safety and efficacy of ginkgo in nursing mothers or infants. In general, it is well tolerated, but occasionally minor symptoms (e.g., headache, nausea, gastrointestinal complaints, allergic skin rashes) occur in those taking the drug. Ginkgo has caused some cases of bleeding in healthy volunteers caused by its antiplatelet activity. Because there is no published experience with ginkgo during breastfeeding, an alternate therapy may be preferred, especially while nursing a newborn or preterm infant.[1] Dietary supplements do not require extensive pre-marketing approval from the U.S. Food and Drug Administration. Manufacturers are responsible to ensure the safety, but do not need to the safety and effectiveness of dietary supplements before they are marketed. Dietary supplements may contain multiple ingredients, and differences are often found between labeled and actual ingredients or their amounts. A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed information #about dietary supplements# is available elsewhere on the LactMed Web site.
Iodide ion while Breastfeeding
CAS Number: 7553-56-2
Iodine is an essential trace nutrient for all infants that a normal component of breastmilk. Infant requirements are estimated to be 15 mcg/kg daily in fullterm infants and 30 mcg/kg daily in premature infants.[1] Systematic reviews and studies on iodine nutrition found that iodine in breastmilk is adequate in iodine-sufficient countries, but in countries with iodine fortification of foods, many mothers did not obtain adequate iodine and that additional supplementation was desirable.[2][3][4][5] In iodine-deficient areas, supplementation of breastfeeding mothers with iodine appears to be more effective than direct supplementation of the infant in reducing infant iodine deficiency.[6] The American Thyroid Association recommends that breastfeeding women should supplement their diet with a daily oral supplement that contains 150 mcg of iodine, but sustained iodine intake while breastfeeding that exceeds 500 to 1100 mcg daily should be avoided.[7] A survey in the United States between 2011 and 2014 found that only 19% of lactating women used a dietary supplement that contained iodine.[8] The use of excessive amounts of iodine in the mother near term and during breastfeeding (e.g., seaweed soup) can increase breastmilk iodine levels and cause transient hypothyroidism in breastfed infants. The absorption of iodine can be marked after application to open wounds or mucous membranes. Exposure of mothers to unnecessary iodine who are or will be breastfeeding should be avoided or minimized to the extent possible by avoiding its use on maternal mucous membranes (e.g., vaginal use, wound therapy), avoiding prolonged contact time, avoiding repeated applications, and applying it to the smallest possible surface areas of the body. It is possible that maternal exposure to iodine near term could interfere with thyroid studies done as a part of newborn screening tests.
Lidocaine while Breastfeeding
CAS Number: 137-58-6
Lidocaine concentrations in milk during continuous IV infusion, epidural administration and in high doses as a local anesthetic are low and the lidocaine is poorly absorbed by the infant. Lidocaine is not expected to cause any adverse effects in breastfed infants. No special precautions are required.[1][2][3] Lidocaine labor and delivery with other anesthetics and analgesics has been reported by some to interfere with breastfeeding. However, this assessment is controversial and complex because of the many different combinations of drugs, dosages and patient populations studied as well as the variety of techniques used and deficient design of many of the studies. Overall it appears that with good breastfeeding support epidural lidocaine with or without fentanyl or one of its derivatives has little or no adverse effect on breastfeeding success.[4][5][6][7][8] Labor pain medication may delay the onset of lactation.
Oligo Bio Iodine 60 Ml Breastfeeding Analsys - 3
Copper and Breastfeeding
SafeIn most cases, it is okay to take mineral supplements like iron, calcium and copper. These have not been known to affect breast milk levels. However, taking large amounts of a dietary supplement while breast-feeding may be harmful to the mother and/or baby and should be avoided.
What should I do if I am breastfeeding mother and I am already exposed to Oligo Bio Iodine 60 Ml?
Due to high dilution of ingredients in homeopathic medicines they do not create much problem for baby. Oligo Bio Iodine 60 Ml is a homeopathic medicine and if your baby does not have any abnormal symptoms then there is nothing to worry about. Be careful with too much usage of ethanol based homeopathic medicines during breastfeeding.
I am nursing mother and my doctor has suggested me to use Oligo Bio Iodine 60 Ml, is it safe?
Homeopathic medicines are usually safe in breastfeeding and if Oligo Bio Iodine 60 Ml has been recommended by doctor then there should be no concern about its usage in breastfeeding.
If I am using Oligo Bio Iodine 60 Ml, will my baby need extra monitoring?
Not exactly.
Who can I talk to if I have questions about usage of Oligo Bio Iodine 60 Ml in breastfeeding?
US
National Womens Health and Breastfeeding Helpline: 800-994-9662 (TDD 888-220-5446) 9 a.m. and 6 p.m. ET, Monday through Friday
UK
National Breastfeeding Helpline: 0300-100-0212 9.30am to 9.30pm, daily
Association of Breastfeeding Mothers: 0300-330-5453
La Leche League: 0345-120-2918
The Breastfeeding Network supporter line in Bengali and Sylheti: 0300-456-2421
National Childbirth Trust (NCT): 0300-330-0700
Australia
National Breastfeeding Helpline: 1800-686-268 24 hours a day, 7 days a week
Canada
Telehealth Ontario for breastfeeding: 1-866-797-0000 24 hours a day, 7 days a week
