American Academy of Pediatrics and other medical experts exclusively recommend to breastfeed the baby for first 6 months. Once you introduce baby to other foods it is recommended to breastfeed for at least first year of babys life. Taking medication while breastfeeding could be tricky as most drugs pass in breast milk. In this article we will evaluate Pravastatin Sodium Tablet for its safety in breastfeeding.
What is Pravastatin Sodium Tablet used for?
Therapy with pravastatin sodium tablets should be considered in those individuals at increased risk for atherosclerosis-related clinical events as a function of cholesterol level, the presence or absence of coronary heart disease, and other risk factors. Primary Prevention of Coronary Events In hypercholesterolemic patients without clinically evident coronary heart disease, pravastatin sodium is indicated to: Reduce the risk of myocardial infarction Reduce the risk of undergoing myocardial revascularization procedures Reduce the risk of cardiovascular mortality with no increase in death from non-cardiovascular causes. Hyperlipidemia Pravastatin sodium tablets are indicated as an adjunct to diet to reduce elevated Total-C, LDL-C, Apo B, and TG levels and to increase HDL-C in patients with primary hypercholesterolemia and mixed dyslipidemia (Fredrickson Type IIa and IIb).8 Pravastatin sodium tablets are indicated as adjunctive therapy to diet for the treatment of patients with elevated serum triglyceride levels (Fredrickson Type IV). Pravastatin sodium tablets are indicated for the treatment of patients with primary dysbetalipoproteinemia (Fredrickson Type III) who do not respond adequately to diet. Pravastatin sodium tablets are indicated as an adjunct to diet and life-style modification for treatment of HeFH in children and adolescent patients ages 8 years and older if after an adequate trial of diet the following findings are present. LDL-C remains ≥190 mg/dL or LDL-C remains ≥160 mg/dL and; there is a positive family history of premature cardiovascular disease or two or more other CVD risk factors are present in the patient. Lipid-altering agents should be used in addition to a diet restricted in saturated fat and cholesterol when the response to diet and other nonpharmacological measures alone has been inadequate (see NCEP Guidelines below). Prior to initiating therapy with pravastatin, secondary causes for hypercholesterolemia (e.g., poorly controlled diabetes mellitus, hypothyroidism, nephrotic syndrome, dysproteinemias, obstructive liver disease, other drug therapy, alcoholism) should be excluded, and a lipid profile performed to measure Total-C, HDL-C, and TG. For patients with triglycerides (TG) <400 mg/dL (<4.5 mmol/L), LDL-C can be estimated using the following equation: LDL-C = Total-C - HDL-C - 1/5 TG For TG levels >400 mg/dL (>4.5 mmol/L), this equation is less accurate and LDL-C concentrations should be determined by ultracentrifugation. In many hypertriglyceridemic patients, LDL-C may be low or normal despite elevated Total-C. In such cases, HMG-CoA reductase inhibitors are not indicated. Lipid determinations should be performed at intervals of no less than four weeks and dosage adjusted according to the patient’s response to therapy. The National Cholesterol Education Program’s Treatment Guidelines are summarized below: Table 5: NCEP Treatment Guidelines: LDL-C Goals and Cutpoints for Therapeutic Lifestyle Changes and Drug Therapy in Different Risk Categories Risk Category LDL Goal (mg/dL) LDL Level at Which to Initiate Therapeutic Lifestyle Changes (mg/dL) LDL Levels at Which to Consider Drug Therapy (mg/dL) CHDCHD, coronary heart disease. or CHD Risk equivalents(10-year risk >20%) <100 ≥100 ≥130(100-129: drug optional)Some authorities recommend the use of LDL-lowering drugs in this category if an LDL- C level of <100 mg/dL cannot be achieved by therapeutic lifestyle changes. Others prefer use of drugs that primarily modify triglycerides and HDL-C, e.g., nicotinic acid or fibrate. Clinical judgement also may call for deferring drug therapy in this subcategory. 2+ Risk factors (10-year risk ≤20%) <130 ≥130 10-year risk 10%-20%:≥130 10-year risk <10%: ≥160 0-1 Risk factorAlmost all people with 0-1 risk factor have 10-year risk <10%; thus, 10-year risk assessment in people with 0-1 risk factor is not necessary. <160 ≥160 ≥190(160-189: LDL-lowering drug optional) After the LDL-C goal has been achieved, if the TG is still ≥200 mg/dL, non-HDL-C (Total-C minus HDL-C) becomes a secondary target of therapy. Non-HDL-C goals are set 30 mg/dL higher than LDL-C goals for each risk category. At the time of hospitalization for an acute coronary event, consideration can be given to initiating drug therapy at discharge if the LDL-C is ≥130 mg/dL (see NCEP Treatment Guidelines, above). Since the goal of treatment is to lower LDL-C, the NCEP recommends that LDL-C levels be used to initiate and assess treatment response. Only if LDL-C levels are not available, should the Total-C be used to monitor therapy. As with other lipid-lowering therapy, pravastatin sodium tablets are not indicated when hypercholesterolemia is due to hyperalphalipoproteinemia (elevated HDL-C). The NCEP classification of cholesterol levels in pediatric patients with a familial history of hypercholesterolemia or premature cardiovascular disease is summarized below: Category Total-C (mg/dL) LDL-C (mg/dL) Acceptable <170 <110 Borderline 170-199 110-129 High ≥200 ≥130
I am breastfeeding mother and I am using Pravastatin Sodium Tablet. Can it have any bad effect on my kid? Shall I search for better alternative?
As Pravastatin Sodium Tablet is made of only Pravastatin sodium, and Pravastatin sodium is unsafe to use in breastfeeding we can safely reach on conclusion that Pravastatin Sodium Tablet is also unsafe to use while breastfeeding. Below is detailed analysis of Pravastatin sodium and Pravastatin Sodium Tablet during location. We recommend you to go through provided detailed analysis as below take decision accordingly. We also recommend you talk to your health care provider before making final decision.
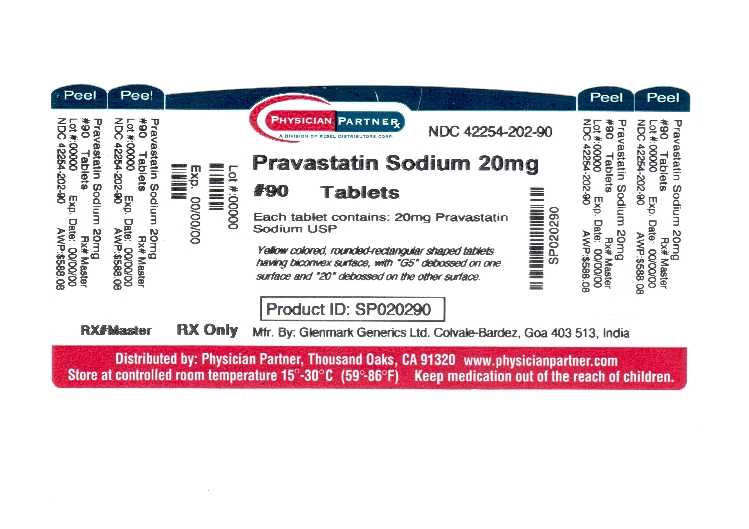
Statement of Manufacturer/Labeler about breastfeeding usage
Nursing mothers A small amount of pravastatin is excreted in human breast milk. Because of the potential for serious adverse reactions in nursing infants, women taking pravastatin sodium should not nurse (see CONTRAINDICATIONS ).
Pravastatin Sodium Tablet Breastfeeding Analsys
UnsafeCAS Number: 81093-37-0
Statin drugs do its action by inhibiting cholesterol synthesis. On latest update relevant data on breastfeeding was not found. Its high plasma protein binding makes excretion into breast milk unlikely. Ability to alter fat composition of breast milk is unknown which is important since infants are in need of high cholesterol intake for adequate brain development, cell membrane building and hormone and vitamin synthesis. Avoid taking it at least while exclusive breastfeeding. Atorvastatin is possibly the safest statin drug because a higher molecular weight that lowers excretion into breast milk even more extensively. For Pravastatin a minimal excretion has been reported. Simvastatin has a lowest oral bioavailability. Avoiding drug treatment for cholesterol as long as breastfeeding is desired would probably not harm long term result of disease. Continuing with a low fat containing diet is recommended.
Pravastatin Sodium Tablet Breastfeeding Analsys - 2
CAS Number: 81093-37-0
Levels of pravastatin in milk are low, but no relevant published information exists with its use during breastfeeding. The consensus opinion is that women taking a statin should not breastfeed because of a concern with disruption of infant lipid metabolism. However, others have argued that children homozygous for familial hypercholesterolemia are treated with statins beginning at 1 year of age, that statins have low oral bioavailability, and risks to the breastfed infant are low, especially with rosuvastatin and pravastatin.[1] Until more data become available, an alternate drug may be preferred, especially while nursing a newborn or preterm infant.
I already used Pravastatin Sodium Tablet and meanwhile I breastfed my baby should I be concerned?
If you observer abnormal behavior or any other health issue in infant then you should immediately call 911 or contact other contact other emergency service provider in your area otherwise closely monitor the baby and inform your doctor about your Pravastatin Sodium Tablet usage and time interval of breastfeeding.
I am nursing mother and my doctor has suggested me to use Pravastatin Sodium Tablet, is it safe?
If your doctor knows that you are breastfeeding mother and still prescribes Pravastatin Sodium Tablet then there must be good reason for that as Pravastatin Sodium Tablet is considered unsafe, It usually happens when doctor finds that overall advantage of taking outweighs the overall risk.
If I am using Pravastatin Sodium Tablet, will my baby need extra monitoring?
Yes, Extra monitoring is required if mother is using Pravastatin Sodium Tablet and breastfeeding as it is considered unsafe for baby.
Who can I talk to if I have questions about usage of Pravastatin Sodium Tablet in breastfeeding?
US
National Womens Health and Breastfeeding Helpline: 800-994-9662 (TDD 888-220-5446) 9 a.m. and 6 p.m. ET, Monday through Friday
UK
National Breastfeeding Helpline: 0300-100-0212 9.30am to 9.30pm, daily
Association of Breastfeeding Mothers: 0300-330-5453
La Leche League: 0345-120-2918
The Breastfeeding Network supporter line in Bengali and Sylheti: 0300-456-2421
National Childbirth Trust (NCT): 0300-330-0700
Australia
National Breastfeeding Helpline: 1800-686-268 24 hours a day, 7 days a week
Canada
Telehealth Ontario for breastfeeding: 1-866-797-0000 24 hours a day, 7 days a week