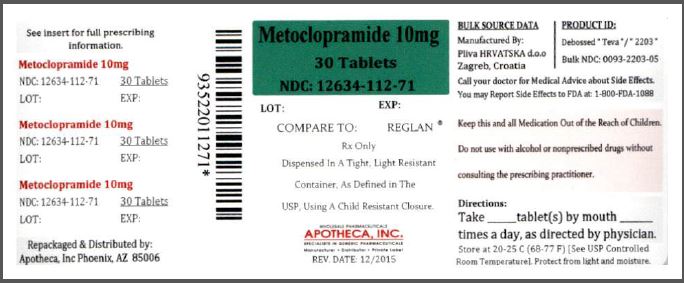
Metoclopramide Tablet while Breastfeeding
What is Metoclopramide Tablet used for?
Is Metoclopramide Tablet usage safe while breastfeeding? If a lactating mother is using it can there be any effect on growth or development of infant?

Nursing Mothers Metoclopramide is excreted in human milk. Caution should be exercised when metoclopramide is administered to a nursing mother.
Metoclopramide Tablet Breastfeeding Analsys
Metoclopramide while Breastfeeding
SafeCAS Number: 364-62-5
Low excreted into breast milk. Not harmful effect on the infant but rare mild intestinal complaints has been reported. At dose of 10 mg three-times-a-day for 2 to 4 weeks an increase of milk production by enhancing Prolactin release has been shown only on low producing Prolactin women. Other well-designed studies have failed to show that effect. Neurological side effect mostly at high dose or long-term use (longer than one month) may occur specially if combined with antidepressant medication. Domperidone has less neurological side effects. The best kind of galactogogue is a breastfeeding on demand with an appropriate nursing technique. Do not use galactogogue substances without a medical supervision.
Metoclopramide Tablet Breastfeeding Analsys - 2
Metoclopramide while Breastfeeding
CAS Number: 364-62-5
Metoclopramide is excreted in variable amounts in breastmilk. Most infants would receive less than 10% of the maternal weight-adjusted dosage, but some receive doses that achieve pharmacologically active serum levels, elevated serum prolactin and possible gastrointestinal side effects. Although most studies have found no adverse effects in breastfed infants during maternal metoclopramide use, many did not adequately observe for side effects. Metoclopramide is used as a galactogogue.[1] Metoclopramide increases serum prolactin. A meta-analysis of 5 placebo-controlled studies concluded that 2 weeks of metoclopramide caused no increase of serum prolactin over placebo, but 3 weeks of treatment did.[2] The clinical value of metoclopramide in increasing milk supply is questionable. Galactogogues should never replace evaluation and counseling on modifiable factors that affect milk production.[3] In well-designed studies that evaluated the effectiveness of metoclopramide as a galactogogue in women who continue to have difficulty producing milk after nursing techniques have been optimized, it was of no additional benefit. Prophylactic use in the mothers of preterm infants has also shown little or no benefit. Metoclopramide has no officially established dosage for increasing milk supply. Most studies have used metoclopramide in a dosage of 10 mg 2 or 3 times daily for 7 to 14 days. Some studies used a tapering dosage for the last days few of the regimen to avoid an abrupt drop in milk supply after drug discontinuation. No published literature supports the efficacy or safety of higher dosages, longer treatment periods or repeated courses of therapy. Postpartum mothers are at a relatively high risk for postpartum depression and metoclopramide can cause depression as a side effect. Therefore, metoclopramide should probably be avoided in women with a history of major depression and not used for prolonged periods in any mothers during this time of high susceptibility.[4][5] Long-term uses of metoclopramide also increases the risk of tardive dyskinesia.[6] Other reported side effects in nursing mothers include tiredness, nausea, headache, diarrhea, dry mouth, breast discomfort, vertigo, restless legs, intestinal gas, hair loss and anxiety.[5][7][8] In a survey of nursing mothers in the United States, 32 had used metoclopramide as a galactogogue and all reported having experienced an adverse reaction from the drug.[9] A larger survey of women taking metoclopramide for lactation enhancement found that 4.8% of women had either palpitations or racing heart rate, 12% reported depression, and 1 to 7% reported other central nervous system side effects ranging from dizziness and headache to involuntary grimacing and tremors. Diarrhea, irritability and fatigue were also relatively common.[10]
I am nursing mother and I have already used Metoclopramide Tablet, what should I do?
Metoclopramide Tablet is safe in breastfeeding and should not create any health problem for your baby but in case you feel any health issue associated with Metoclopramide Tablet you should contact your doctor or health care provider. Be it pregnancy or lactation you shall keep your doctor informed.
I am nursing mother and my doctor has suggested me to use Metoclopramide Tablet, is it safe?
Definitely, Metoclopramide Tablet is safe in lactation for baby. No wonder your doctor has recommended it.
If I am using Metoclopramide Tablet, will my baby need extra monitoring?
No extra baby monitoring required while mother is using Metoclopramide Tablet
Who can I talk to if I have questions about usage of Metoclopramide Tablet in breastfeeding?
US
National Womens Health and Breastfeeding Helpline: 800-994-9662 (TDD 888-220-5446) 9 a.m. and 6 p.m. ET, Monday through Friday
UK
National Breastfeeding Helpline: 0300-100-0212 9.30am to 9.30pm, daily
Association of Breastfeeding Mothers: 0300-330-5453
La Leche League: 0345-120-2918
The Breastfeeding Network supporter line in Bengali and Sylheti: 0300-456-2421
National Childbirth Trust (NCT): 0300-330-0700
Australia
National Breastfeeding Helpline: 1800-686-268 24 hours a day, 7 days a week
Canada
Telehealth Ontario for breastfeeding: 1-866-797-0000 24 hours a day, 7 days a week
