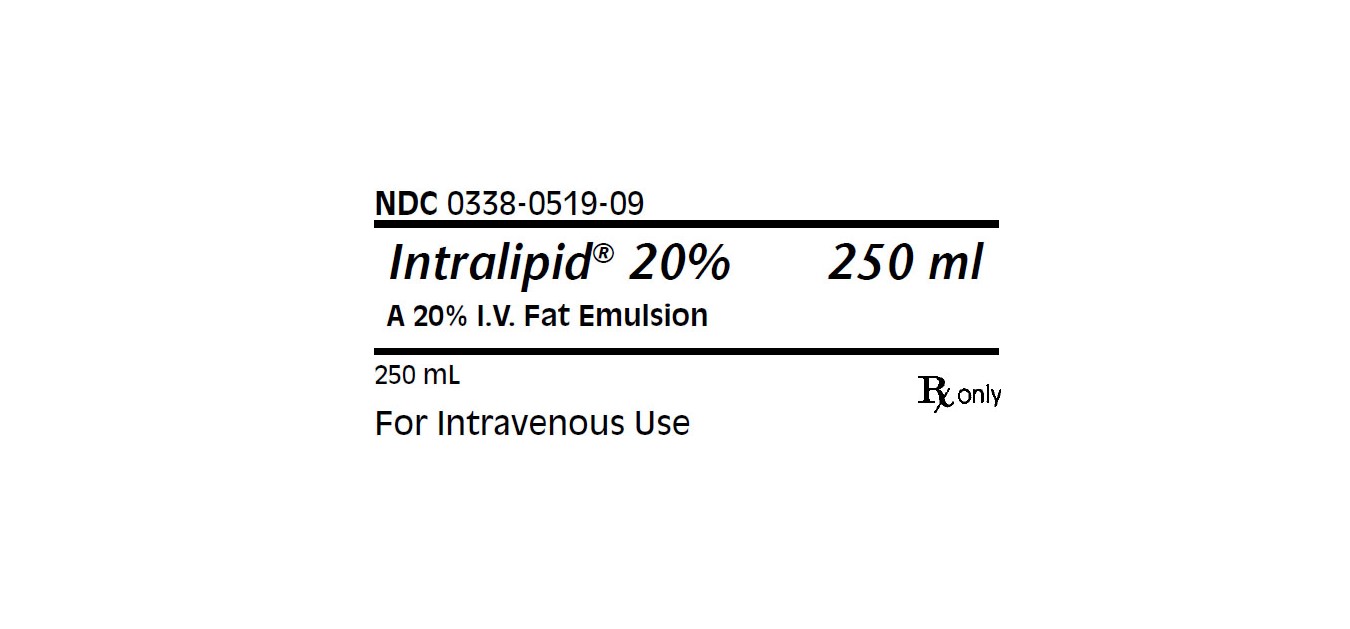
Intralipid Emulsion while Breastfeeding
What is Intralipid Emulsion used for?
Is Intralipid Emulsion usage safe while breastfeeding? If a lactating mother is using it can there be any effect on growth or development of infant?

Intralipid Emulsion Breastfeeding Analsys
Soybean oil while Breastfeeding
Low RiskCAS Number: 8001-22-7
Seeds, oil and extracts of this plant contain Lecithin and Isoflavones like Genistein, Glycitein and Daidzein. Lecithin is formed by phospholipids with hypolipidemic properties (see particular information on LECITHIN). Isoflavones are phytoestrogens which is a property that is being used for treatment of hyperlipidemias and disorders related to menopause. Ingestion of soy derived products by nursing mothers may be a cause of increase concentration in the mother’s plasma, breast milk and infant’s urine. Despite of that soy has been consumed from ancient times by Asian population and could offer some benefit for the welfare, it may act as hormonal disruptor on the endocrine system, especially is the product contains Bisphenol, hence, high exposition during infancy should be avoided. Therefore, it is not recommended an extensive consumption of it while breastfeeding since estrogens may decrease, at least theoretically, the milk production.

What if I already have used Intralipid Emulsion?
Intralipid Emulsion is in the category of low risk, if you have already used it then its not a big deal if health and behavior of baby is good. However your health care provider shall be aware of the fact that you have used Intralipid Emulsion so you should inform him based on your convenience.
I am nursing mother and my doctor has suggested me to use Intralipid Emulsion, is it safe?
Though Intralipid Emulsion dose not comes in category of safe drugs rather it comes in category of low risk but if your doctor is aware that you are breastfeeding your baby and has still recommended it then its advantages must be outweighing the risks.
If I am using Intralipid Emulsion, will my baby need extra monitoring?
Not much monitoring required while using Intralipid Emulsion
Who can I talk to if I have questions about usage of Intralipid Emulsion in breastfeeding?
US
National Womens Health and Breastfeeding Helpline: 800-994-9662 (TDD 888-220-5446) 9 a.m. and 6 p.m. ET, Monday through Friday
UK
National Breastfeeding Helpline: 0300-100-0212 9.30am to 9.30pm, daily
Association of Breastfeeding Mothers: 0300-330-5453
La Leche League: 0345-120-2918
The Breastfeeding Network supporter line in Bengali and Sylheti: 0300-456-2421
National Childbirth Trust (NCT): 0300-330-0700
Australia
National Breastfeeding Helpline: 1800-686-268 24 hours a day, 7 days a week
Canada
Telehealth Ontario for breastfeeding: 1-866-797-0000 24 hours a day, 7 days a week
