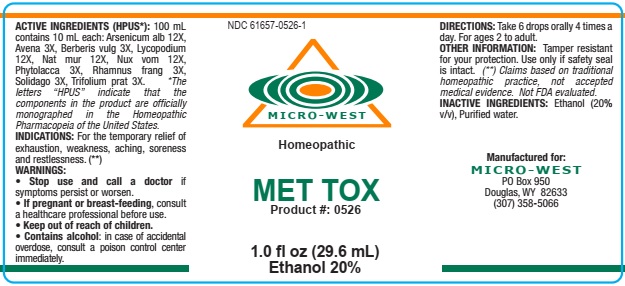
Met-tox while Breastfeeding
What is Met-tox used for?
Brief: FOR THE TEMPORARY RELIEF OF EXHAUSTION, WEAKNESS, ACHING, SORENESS AND RESTLESSNESS
Is Met-tox usage safe while breastfeeding? If a lactating mother is using it can there be any effect on growth or development of infant?

Met-tox Breastfeeding Analsys
Arsenic trioxide while Breastfeeding
DangerousUsed in the treatment of promyelocitic leukemia in adults.
Avena sativa flowering top while Breastfeeding
SafeThe seeds of this leguminous plant are used. Content: carbohydrates, proteins, saponins, vitamins, minerals . Assigned properties: appetite stimulant, lowering of lipemia and glycemic (Gong 2016).Indications according to Commission E of the German Ministry of Health: Anorexia, Atopic Dermatitis. Widely used as a galactogogue in many cultures around the world (Ayers 2000, Winterfeld 2012, Sim 2013, The Royal Women's .. 2013, Bazzano 2016). Case-control studies looking for evidence on the increment of milk production associated to the use of fenugreek are few (Turkyılmaz 2011, Ghasemi 2015), along with a variety of methodological deficiencies. Other studies have failed to find such an effect with the use of fenugreek (Damanik 2006). Studies with an appropriate design are needed to provide high quality evidence to make clinical recommendations on its use (Forinash 2012, Zapantis 2012, Committee LM AEP 2012, Mortel 2013, Bazzano 2016) A higher antioxidant effect in the breastmilk of women who have consumed mixed infusions containing this or other herbs has not been shown (Kavurt 2013). Given the wide spread use and lack of toxicity of this herb, a moderate consumption would be compatible with breastfeeding, yet high doses may produce hypoglycemia (EMA 2011, Gong 2016) and, because of the odor appearing in the urine of the infant, a lab test may be required to make a differential diagnosis with maple syrup disease of the newborn (Sewell 1999, Korman 2001). Avoid the use of a galactogogue without a sanitary control. Best galactagogue results are achieved through on-demand breastfeeding along with an adequate technique in a mother who is able to maintain self-confidence (ABM 2011, Mannion 2012). Precautions when taking plant preparations: 1. Ensure that they are from a reliable source: poisoning has occurred due to confusing one plant with another with toxic properties, as well as poisoning from heavy metals extracted from the ground and food poisoning due to contamination with bacteria or fungi. 2. Do not take in large amounts; follow recommendations from professional experts in phytotherapy. "Natural" products are not always good in any quantity: plants contain active substances from which much of our traditional pharmacopoeia has been obtained and can result in poisoning or act as endocrine disruptors if taken in excessive amounts or time periods.
Berberis vulgaris root bark while Breastfeeding
DangerousCAS Number: 84649-92-3
Roots and bark are used. It contains Berberine that may be a cause of gastritis, nephritis, phototoxicity and severe jaundice by displacement of albumin -linked bilirubin: higher risk of kernicterus to newborns, which is greater in cases of 6-Glucose-PD deficiency. It is popularly widely used, however, its effectiveness has not been shown. Use not approved by the Commission E of German Ministry of Health. It should be avoided.
Lycopodium clavatum spore while Breastfeeding
UnsafeAerial summits and spores of this fern are used. Traditionally use as a diuretic and intestinal spasm relief drug. Also used for abrasions and skin irritation. It may be a cause of asthma and contact dermatitis.
Sodium chloride while Breastfeeding
SafeCAS Number: 7647-14-5
Sodium chloride either as cooking salt, or, as oral rehydration solution, or, as IV fluid, is entirely compatible with BF.
Strychnos nux-vomica seed while Breastfeeding
DangerousCAS Number: 8046-97-7
Dried seed of this plant has been used. It contains brucine and strychnine. It is highly toxic and easily lethal.
Solidago virgaurea flowering top while Breastfeeding
SafeCAS Number: 85117-06-2
Perennial plant. Florid summits are used.It contains flavonoids, tannins, saponosides.Indication after Commission E of German Ministry of Health: diuretic. Daily dose: 6 to 12 g of drug or equivalent. Be cautious with extracted alcohol and tincture.
Iron while Breastfeeding
SafeSeveral ferrous salts of iron (ascorbate, aspartate, citrate, chloride, fumarate, gluconate, lactate, oxalate, succinate, sulfate, glycine sulfate, etc.) are used in oral administration for treating or preventing iron deficiency anemia.Its molecular weight varies from 170 for the fumarate and succinate, and from 280 for lactate and sulfate to 400 for aspartate and ascorbate. Characteristics of iron metabolism in the body make unlikely that it would be excreted in a significant amount into breast milk.It is a medication used for treatment of Neonatal Anemia in premature babies. Iron is excreted in small amounts in human milk, usually being enough for covering the daily needs of infants due to its high bioavailability. There is no correlation between mother's daily intake of iron and its concentration in breast milk.Iron supplementation to the mother does not increase levels of iron in breast milk or infant plasma significantly. Excessive supplementation can reduce the zinc concentration in milk. WHO List of Essential Medicines 2002: compatible with breastfeeding.
Chromium while Breastfeeding
SafeCAS Number: 7440-47-3
Heavy metal that in its trivalent oxidative states (3+) has a great nutritional value since it acts as a trace element (trace element) that enhances the action of insulin and is involved in the metabolism of carbohydrates, fats and proteins. Meat, seafood, brewer's yeast, whole grains and nuts (especially walnuts), among others, are very rich in chromium. The recommended intake in nursing mothers is 45 micrograms daily (Ares Segura 2015). The average concentration of chromium in breast milk is 1 nanogram / mL, ranging between 0.2 and 7 ng / mL and is independent of plasma levels and maternal daily intake (Kumpulainen 1980, Anderson 1993, Mohamedshah 1998). With a varied and balanced diet not mineral supplements are needed. Excessive intake of chromium can cause skin problems in infants (Adachi 2007). No increased concentrations of chromium in milk or problems in breastfed by mothers with hip containing chromium in its composition (Nelis 2013, Oppermann 2015) Not to be confused with states hexavalent (6+) industrial and irritating, toxic and carcinogenic effects (see tab chromic acid or chromium trioxide).
Calcium while Breastfeeding
SafeCAS Number: 471-34-1
Various calcium salts (Acetate, Carbonate, Chloride, Citrate, Phosphate, Gluceptate, Glucobionato, Lactate, Laxctobionato Pidolate, Silicate) are used in the management of hypocalcemia, supplements for treating calcium deficiency states and antacids ( Carbonate and Silicate) Daily requirement of calcium during lactation are 1 g (1.3 g in children under 20 years).Calcium supplements in the diet does not affect the concentration of calcium in milk.Excessive intake of calcium is not good for health. During lactation, consumption of calcium should not exceed 2.5 g a day. WHO List of Essential Medicines 2002 states that it is compatible with breastfeeding.
Activated charcoal while Breastfeeding
SafeCAS Number: 7440-44-0
Powdered carbon with high adsorption levels.Administrated orally, it adsorbs drugs and toxins, avoiding their absorption from the gastrointestinal tract. It also has uses as an antidiarrheal and antiflatulent and for marking breast lesions in mammography. Since the last update we have not found published data about its excretion in breast milk. Its zero intestinal absorption (Torbet 2005, AEMPS 1998) prevents its passing into plasma and therefore into breast milk. It use is permitted in infants under one year old (Pediamecum 2015).
Selenium while Breastfeeding
Low RiskCAS Number: 7782-49-2
Essential trace element necessary for the functioning of the glutathione-peroxidase enzyme system that protects cellular structures from oxidative damage. It is obtained from foods such as vegetables, cereals, legumes, garlic, fish, seafood, eggs and meat. The amount of selenium in these sources depends on the concentration of selenium in the soil. The brazil nut (Bertholletia excelsa) is the food with the highest known concentrations of selenium. Selenium deficiency is very rare. With a staple diet it is not necessary to take selenium supplements in the absence of disease or a condition that may warrant it: parenteral nutrition, Crohn's disease, prematurity (MedlinePlus 2017). Taking too much selenium can cause selenosis, a condition that causes dermatological symptoms (alopecia, nail dystrophy), digestive symptoms, neurological symptoms and fatigue (MedlinePlus 2017).Nutritional supplements containing excessive amounts of selenium have resulted in severe poisoning (Aldosary 2012, Senthilkumaran 2012).The potential effects of selenium on cancer prevention, cardiovascular disease, and heavy metal poisoning and toxins are not proven, so supplementation of selenium other than from normal diet is not recommended (MedlinePlus 2017). The daily needs of selenium for breastfeeding mothers are 70-75 micrograms (mcg) daily. In infants it is 2 to 3 mcg/kg (10 mcg/day during the first 4 months) with a maximum of 30 mcg/day (MedlinePlus 2017, Kipp 2015). Selenium is found naturally in milk in its organic form of selenomethionine (Dorea 2002). The amount of selenium in colostrum is 80 mcg per litre and in mature milk 12-20 mcg/L, with no or very weak correlation with plasma selenium levels or daily intake of selenium (Wasowicz 2001, Bianchi 1999, Artaud 1993, Cummings 1992, Levander 1987, Higashi 1983). However, there are authors who find that selenium supplements for breastfeeding mothers increase selenium levels in milk and infants may exceed their daily needs for selenium. (Dorea 2002, Trafikowska 1996). Better plasma levels of selenium have been found in breastfed infants than in formula-fed infants (Strambi 2004, Sorvacheva 1996). There are lower plasma levels of selenium in babies born small for their gestational age (Strambi 2004).
Zinc while Breastfeeding
SafeZinc (Zn) is an essential element for nutrition. It is present in many foods.Recommended daily allowance of Zn is 8 to 15 mg. (Moran Hall 2010). Millions of people worldwide are Zn-deficient.It is used as a treatment for Wilson's disease and Acrodermatitis Enteropathica. Zn is involved in the regulation process of lactation (Lee 2016).Pasteurization of the milk does not affect the concentration of Zn and other trace elements (Mohd Taufek-2016). The average concentration of Zn in breastmilk is 4 to 16 mg / L (Picciano 1976, Hannan 2005, Dórea 2012) which is independent of plasma levels and maternal daily intake (Krebs 1995, Chierici 1999, Hannan 2009).Intestinal absorption of zinc is almost doubled during pregnancy and lactation (Fung 1997).Zinc levels in the infant are dependent on Zinc levels in the breast milk (Dumrongwongsiri 2015)With a varied and balanced diet, an extra intake of minerals is not needed. Excessive intake of Zinc may cause gastrointestinal problems and Pancytopenia (Irving 2003).
Cobalt while Breastfeeding
SafeCAS Number: 7440-48-4
Gray powder or metal, odorless. There is a risk of asthma crisis if cobalt powder is inhaled. It can be a cause of skin, ocular and respiratory tract irritation. Acetate, sulfate, trioxide and nitrate cobalt salts are potentially carcinogenic. Mandatory measures to prevent inhalation (room air extraction and respiratory protection) and ingestion (avoid eating, drinking or smoking in the work place). The industry must ensure a Threshold Limit Value (TLV) (TWA as well) less than 0.05 mg/m3 (cobalt salts less than 0.002 mg/m3). Biological Exposition Index (BEI) on the last labor week day: 15 micrograms/L in the urine, 1 microgram/L in the blood. Benefits of breastfeeding are largely more important than risk related to the presence of mild level environment pollutants in human milk, in many instances, they are at lower content than those found in cow’s milk or other foods. (Codex alimentarius FAO-WHO).
Arsenic while Breastfeeding
DangerousUsed in the treatment of promyelocitic leukemia in adults.
Strontium while Breastfeeding
DangerousIt has a too long half-life span (51 days). Used in the treatment of pain secondary to bone metastasis of cancer.
Lead while Breastfeeding
UnsafeCAS Number: 7439-92-1
It is an environmental contaminant. As a heavy metal it is found in excess in products like paintings, fuel and metal industry. Certain make-ups, infusion herbals, meat from chased animals and ceramic made pottery may increase the risk of exposure. It can be stored in soft tissues for one month and in bones for decades. Removing of lead from bones occurs during pregnancy and lactation leading to an increase in the serum many years after exposure. It can cause cardiovascular and respiratory toxicity. More intensively it affects infants and children it may cause neurologic damage. Maximal accepted levels by international agencies like WHO, CDC, EFSA – even though a 0 level is desirable – are: 10 mcg/L in water, 5 mcg/L in breast milk and an ingestion of 2.5 mcg/k/d for infants less of 6 months of age. Absorption through the lungs is 50% and through the gut is less than 10%. In blood of unexposed persons serum levels should not be higher than 10 mcg/dL. Working mothers at fertile age showing a lead serum level higher than 30 mcg/dL should be removed from work place. Working pregnant or nursing women should be removed from places with high risk of toxin exposition (Regulated by EU Council Law/85/ from 19.10.1992). Mothers should not breastfeed if they are found to be intoxicated or contaminated. Same recommendation is suitable for mothers who undergo a chelating treatment (since lead is removed from bones and let free). Blood and breast milk testing is highly recommended to have lead level measured. Mothers should avoid nursing whenever lead level is higher than 16 mcg/L in the milk or 16 mcg/dL in the serum. (Lead levels in the milk are usually 10% of those in the serum). Benefits of breastfeeding widely overcome those issues related to the presence of low level environmental contaminants in human milk that in many instances are lower than those present in cow’s milk based products and other food. (Codex alimentarius FAO-WHO). Published papers from studies done on this matter have shown higher lead levels contained in powdered artificial milks than in human milk.
Chloride ion while Breastfeeding
SafeCAS Number: 7647-14-5
Sodium chloride either as cooking salt, or, as oral rehydration solution, or, as IV fluid, is entirely compatible with BF.
Lithium while Breastfeeding
UnsafeCAS Number: 554-13-2
It is excreted into breast milk in amounts that may be clinically significant and can be as high as a half of that reached in mother’s plasma and up to one third of the therapeutic level in the infant. In infants and newborns (5 days), premature babies and dehydrated or infected infants, who may show reduced clearance mechanisms for lithium, there have been reports of clear signs of lithium toxicity caused by ingestion of breast milk: cyanosis, lethargy, hypotonia or slight increase in TSH. However, there are numerous cases of infants whose mothers were on lithium who did not show any clinical, growth or neurodevelopmental problem at the short or long term. Breastfeeding is less risky for healthy term infants whose mothers are treated with lithium when she or her family has capacity enough to monitor the occurrence of adverse effects, medical supervision and, whenever necessary, monitoring of lithium levels in the mother-infant dyad. Mothers should stop taking lithium 1 to 2 days before delivery or cesarean section in order to decrease plasma levels in the newborn. Lithium may be, or not, a cause of increased Prolactin and galactorrhea.
Bromine while Breastfeeding
Low RiskCAS Number: 7726-95-6
It is naturally found as a bromide, and, industrially used on processing fuels, natural gas, photography fluids, and as a tranquilizer (not longer recommended). Bromide liberates a red steam that is irritant and may enter the breast milk. Eczema and somnolence have been described. Mothers who would be labor exposed (photographic film development) should receive enough ventilation. Monitoring of blood level may be considered. Benefits of breastfeeding are largely more important than risk related to the presence of mild level environment pollutants in human milk, in many instances, they are at lower content than those found in cow’s milk or other foods. (Codex alimentarius FAO-WHO).
Sodium while Breastfeeding
SafeCAS Number: 7647-14-5
Sodium chloride either as cooking salt, or, as oral rehydration solution, or, as IV fluid, is entirely compatible with BF.
Iodine while Breastfeeding
UnsafeCAS Number: 7553-56-2
Disinfectant that contains high amount (2-7%) of Iodine in solution with alcohol or water (Lugol's solution) Not absorbed through intact skin of adults. However, it may trespass the inflamed skin, wounds, mucosa surfaces like vagina, in which case can reach concentration in grams in the human serum (1 g = 1,000 milligrams = 1,000,000 micrograms). Normal daily allowance is considered to be as high as 100 to 150 micrograms that increases to 200 – 300 micrograms in pregnancy or nursing period. The latter means less than one third of a milligram. Iodine is concentrated into breast milk with a level that could reach 20 times higher than the concentration in the blood. It has been found higher levels of Iodine, altered results of neonatal screening test for thyroid function, and, transient hypothyroidism in infants whose mothers were exposed to Iodine Povidone. Use should be avoid in the Delivery Room, Operating Room (C-section), Neonatal Units, Toddler admision areas and during the breastfeeding period. Sporadic or inadvertent use, specially on normal skin, does not require special test or procedures because it does not pose higher risk to the child.
Gadolinium while Breastfeeding
SafeThe various contrast media that are gadolinium derivatives and used for explorations with Magnetic Resonance Imaging (MRI) are considered compatible with breastfeeding because they are quickly eliminated (elimination half-life of less than 2 hours). They undergo very little metabolic changes and are virtually non-absorbable orally. They are structurally very similar to each other. Some have been shown to have no or minimal excretion into the milk. Less than 0.04% of the dose given to the mother ends just going into the milk.Due to its low oral bioavailability, intestinal absorption should be less than 1% of the dose took by the infant.The maximum dose received by the infant is considered less than 0.0004% of the maternal dose, which is much less than the dose administered to a newborn infant who undergoes a MRI scan. Most Radiology Scientific Societies agree that after an MRI scan is not necessary to temporarily stop breastfeeding. Some authors recommend avoiding the use on lactating women of some Gadolinium contrast media that would pose a high risk for developing Systemic Nephrogenic Fibrosis, especially in the neonatal period, like gadoversetamide, and gadodiamide dimeglumine, by using instead low-risk ones like gadoterate, gadoteridol and gadobutrol. See below the information of this related group:
Fluoride ion while Breastfeeding
SafeCAS Number: 7681-49-4
Used on teeth decay prophylaxis. It is contraindicated if water has been fluorated (>7ppm).
Cadmium while Breastfeeding
Low RiskCAS Number: 7440-43-9
Environmental pollutant. Heavy metal produced by zinc and charcoal mining industry, water plumbing, tobacco smoking, and burning of residual material. Benefits of breastfeeding are largely more important than risk related to the presence of mild level environment pollutants in human milk, in many instances, they are at lower content than those found in cow’s milk or other food. (Codex alimentarius FAO-WHO).
Mercury while Breastfeeding
Low RiskCAS Number: 7439-97-6
Environmental pollutant that is used for manufacturation of batteries, fungicidal products, dental amalgam, and contaminated fish. Most of mercury present in breast milk does it as an inorganic substance which is almost non-absorbable. Breastfeeding should be discontinued whenever a mother is contaminated or intoxicated. It may be a source of neurological troubles. Benefits of breastfeeding are largely more important than risk related to the presence of mild level environment pollutants in human milk, in many instances, they are at lower content than those found in cow’s milk or other foods. (Codex alimentarius FAO-WHO).
Potassium while Breastfeeding
SafeCAS Number: 7447-40-7
Human milk has a potassium concentration of 13 meq/L, almost a half of rehydration solution content and a quarter of maximal IV recommended dose. Potassium supplementation does not alter milk concentration without increasing mother’s serum concentration, which is strictly limited from 3,5 to 5,5 meq/L.
Gallium while Breastfeeding
UnsafeCAS Number: 41183-64-6
Pump-out breast milk and store it in refrigerator for some days before testing. After test is done, dispose milk for:1 week if dose is 7 Mbq (0,2 mCi)2 weeks if dose is 50 Mbq (1,3 mCi)4 weeks if dose is 150 Mbq (4,0 mCi)Keep-on pumping to mantain milk production.Choose the shortest half-life span radionuclide as possible.
Gold while Breastfeeding
Low RiskCAS Number: 7440-57-5
One case of facial edema that was barely related to this drug has been described. It has an extremely long half-life span.
Indium while Breastfeeding
UnsafeCAS Number: 15750-15-9
Pump-out breast milk and keep it in refrigerator for some days before procedure. After test is done, keep-on pumping the breast (to stimulate milk production), and, dispose it for 8 to 24 hours (1 week if dose is 20 Mbq=0,5mCi). Feed the baby with stored milk.(Choose the shortest half-life span radionucleotide as possible)
Silver while Breastfeeding
SafeCAS Number: 7761-88-8
Avoid using it on the breast or cleanse thoroughly before nursing.
Met-tox Breastfeeding Analsys - 2
Arsenic trioxide while Breastfeeding
CAS Number: 1327-53-3
Most sources consider breastfeeding to be contraindicated during maternal antineoplastic drug therapy. It might be possible to breastfeed safely during intermittent therapy with an appropriate period of breastfeeding abstinence; the manufacturer recommends an abstinence period of 1 week after the last dose. Chemotherapy may adversely affect the normal microbiome and chemical makeup of breastmilk.[1] Women who receive chemotherapy during pregnancy are more likely to have difficulty nursing their infant.[2]
Magnesium while Breastfeeding
CAS Number: 3344-18-1
No information is available on the clinical use of magnesium citrate during breastfeeding. However, other magnesium salts have been studied. Intravenous magnesium sulfate increases milk magnesium concentrations only slightly. Oral absorption of magnesium by the infant is poor, so maternal magnesium citrate is not expected to affect the breastfed infant's serum magnesium. Magnesium citrate supplementation during pregnancy might delay the onset of lactation, but it can be taken during breastfeeding and no special precautions are required.
Sulfur while Breastfeeding
CAS Number: 7704-34-9
Sulfur 5% to 10% in a petrolatum base is safe for topical use in children, including infants under 2 months of age.[1] This makes it a useful alternative to organic insecticides for treating scabies in nursing mothers; however, the petrolatum base makes undesirable for use on the breast.
Lithium while Breastfeeding
CAS Number: 554-13-2
Although lithium appears on many lists of drugs contraindicated during breastfeeding, other sources do not consider it an absolute contraindication, especially in infants over 2 months of age and during lithium monotherapy.[1][2][3][4] Numerous reports exist of infants who were breastfed during maternal lithium therapy without any signs of toxicity or developmental problems. Most were breastfed from birth and some continued to nurse for up to 1 year of maternal lithium therapy. Limited data suggest that lithium in milk can adversely affect the infant when its elimination is impaired, as in dehydration or in newborn or premature infants. Neonates may also have transplacentally acquired serum lithium levels. Because maternal lithium requirements and dosage may be increased during pregnancy, maternal serum levels should be monitored frequently postpartum and dosage reduced as necessary to avoid excessive infant exposure via breastmilk.[5] The long-term effects of lithium on infants are not certain, but limited data indicate no obvious problems in growth and development.[6] Lithium may be used in mothers of fullterm infants who are willing and able to monitor their infants. Discontinuing lithium 24 to 48 hours before Cesarean section delivery or at the onset of spontaneous labor and resuming the prepregnancy lithium dose immediately after delivery should minimize the infant's serum lithium concentration at birth.[7] Some investigators recommend monitoring infant serum lithium, serum creatinine, BUN, and TSH in intervals ranging from "periodic" to every 4 to 12 weeks during breastfeeding and maternal lithium therapy.[3][8][9] However, others recommend close pediatric follow-up of the infant and only selective laboratory monitoring as clinically indicated.[7] Breastfeeding should be discontinued immediately and the infant evaluated if the infant appears restless or lethargic or has feeding problems.[7]
Iodine while Breastfeeding
CAS Number: 7553-56-2
Iodine is an essential trace nutrient for all infants that a normal component of breastmilk. Infant requirements are estimated to be 15 mcg/kg daily in fullterm infants and 30 mcg/kg daily in premature infants.[1] Systematic reviews and studies on iodine nutrition found that iodine in breastmilk is adequate in iodine-sufficient countries, but in countries with iodine fortification of foods, many mothers did not obtain adequate iodine and that additional supplementation was desirable.[2][3][4][5] In iodine-deficient areas, supplementation of breastfeeding mothers with iodine appears to be more effective than direct supplementation of the infant in reducing infant iodine deficiency.[6] The American Thyroid Association recommends that breastfeeding women should supplement their diet with a daily oral supplement that contains 150 mcg of iodine, but sustained iodine intake while breastfeeding that exceeds 500 to 1100 mcg daily should be avoided.[7] A survey in the United States between 2011 and 2014 found that only 19% of lactating women used a dietary supplement that contained iodine.[8] The use of excessive amounts of iodine in the mother near term and during breastfeeding (e.g., seaweed soup) can increase breastmilk iodine levels and cause transient hypothyroidism in breastfed infants. The absorption of iodine can be marked after application to open wounds or mucous membranes. Exposure of mothers to unnecessary iodine who are or will be breastfeeding should be avoided or minimized to the extent possible by avoiding its use on maternal mucous membranes (e.g., vaginal use, wound therapy), avoiding prolonged contact time, avoiding repeated applications, and applying it to the smallest possible surface areas of the body. It is possible that maternal exposure to iodine near term could interfere with thyroid studies done as a part of newborn screening tests.
Barium while Breastfeeding
CAS Number: 7727-43-7
Because barium sulfate is not absorbed after oral or rectal administration, it will not enter the milk, reach the bloodstream of the infant or cause any adverse effects in breastfed infants. No special precautions are required.
Gallium while Breastfeeding
CAS Number: 41183-64-6
Information in this record refers to the use of Ga 67 citrate as a diagnostic agent. The United States Nuclear Regulatory Commission states that breastfeeding should be interrupted temporarily after administration of Ga 67 citrate to a nursing mother. The duration of breastfeeding interruption depends on the dose administered (see table).[1] The International Commission on Radiological Protection recommends discontinuation of breastfeeding for more than 3 weeks after Ga 67 citrate.[2] Those receiving the higher doses might have to permanently discontinue breastfeeding this infant.[3][4] After doses greater than 200 MBq, consideration of temporarily limiting close contact between the mother and infant.[5] During the period of interruption, the breasts should be emptied regularly and completely. If the mother has expressed and saved milk prior to the examination, she can feed it to the infant during the period of nursing interruption.[3][5][6] The milk that is pumped by the mother during the time of breastfeeding interruption can either be discarded or[3][6] stored frozen and given to the infant after 10 physical half-lives, or about 33 days, have elapsed. Mothers concerned about the level of radioactivity in their milk could ask to have it tested at a nuclear medicine facility at their hospital. When the radioactivity is at a safe level she may resume breastfeeding. A method for measuring milk radioactivity and determining the time when a mother can safely resume breastfeeding has been published.[4] Mothers who receive a dose less than 190 MBq for an inflammation scan need not refrain from close contact with their infants.[7]
| Dose | Duration of Interruption[1] |
|---|---|
| 150 MBq (4 mCi) | 1 month |
| 50 MBq (1.3 mCi) | 2 weeks |
| 7 MBq (0.2 mCi) | 1 week |
Nitrogen while Breastfeeding
CAS Number: 7727-37-9; 17778-88-
No information is available on the clinical use of liquid nitrogen on the skin during breastfeeding. Because it is a nontoxic gas that is unlikely to appear in breastmilk or be absorbed by the infant, it is considered safe to use during breastfeeding. No special precautions are required.
Met-tox Breastfeeding Analsys - 3
Sulfur and Breastfeeding
SafeNote: Study and data for tropical use only
Warning: Tropical usage in breast area shall be avoided to prevent the Thuja passing orally in Infants.
Copper and Breastfeeding
SafeIn most cases, it is okay to take mineral supplements like iron, calcium and copper. These have not been known to affect breast milk levels. However, taking large amounts of a dietary supplement while breast-feeding may be harmful to the mother and/or baby and should be avoided.
Nitrogen and Breastfeeding
SafeWhat should I do if already breastfed my kid after using Met-tox?
Due to high dilution of ingredients in homeopathic medicines they do not create much problem for baby. Met-tox is a homeopathic medicine and if your baby does not have any abnormal symptoms then there is nothing to worry about. Be careful with too much usage of ethanol based homeopathic medicines during breastfeeding.
I am nursing mother and my doctor has suggested me to use Met-tox, is it safe?
Homeopathic medicines are usually safe in breastfeeding and if Met-tox has been recommended by doctor then there should be no concern about its usage in breastfeeding.
If I am using Met-tox, will my baby need extra monitoring?
Not exactly.
Who can I talk to if I have questions about usage of Met-tox in breastfeeding?
US
National Womens Health and Breastfeeding Helpline: 800-994-9662 (TDD 888-220-5446) 9 a.m. and 6 p.m. ET, Monday through Friday
UK
National Breastfeeding Helpline: 0300-100-0212 9.30am to 9.30pm, daily
Association of Breastfeeding Mothers: 0300-330-5453
La Leche League: 0345-120-2918
The Breastfeeding Network supporter line in Bengali and Sylheti: 0300-456-2421
National Childbirth Trust (NCT): 0300-330-0700
Australia
National Breastfeeding Helpline: 1800-686-268 24 hours a day, 7 days a week
Canada
Telehealth Ontario for breastfeeding: 1-866-797-0000 24 hours a day, 7 days a week
