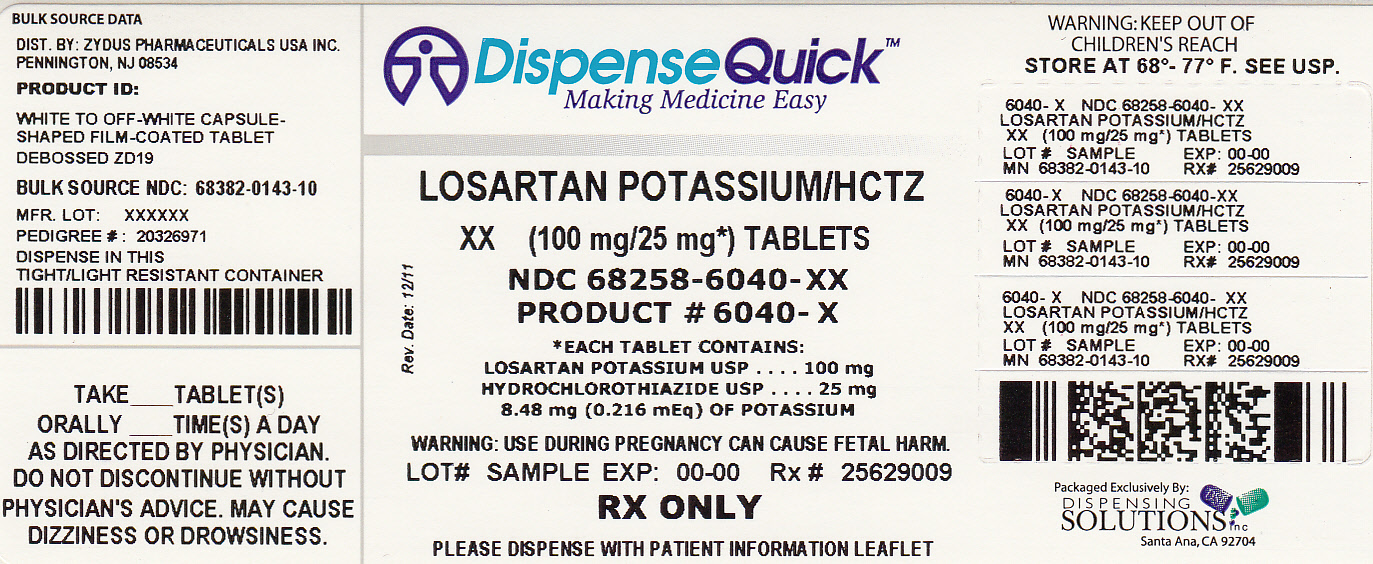
Losartan Potassium And Hydrochlorothiazide Tablet while Breastfeeding
Is using Losartan Potassium And Hydrochlorothiazide Tablet unsafe in breastfeeding? Can there be bad consequences for baby if I use it while breastfeeding?

Losartan Potassium And Hydrochlorothiazide Tablet Breastfeeding Analsys
Hydrochlorothiazide while Breastfeeding
SafeCAS Number: 58-93-5
Thiazide diuretic drug. Excretion into breast milk is clinically non-significant. No side-effects were observed in a one-month old breastfed baby whose mother was treated with this medication. Drug level in the plasma of this child was undetectable. Long-term treatment with diuretic drugs (particularly Thiazide type ones with long-lasting effect and loop-acting mechanism) may inhibit lactation, mostly if lactation is not well-established yet. Use as lower dose as possible, especially during the first postnatal month. American Academy of Pediatrics 2013: Maternal Medication Usually Compatible With Breastfeeding. WHO Model List of Essential Drugs 2002: Compatible with breastfeeding.
Losartan potassium while Breastfeeding
Low RiskCAS Number: 124750-99-8
At latest update, relevant published data on excretion into breast milk were not found. A high protein-binding capacity makes excretion into breast milk unlikely. In addition, a low oral bioavailability makes difficult the absorption towards the infant's plasma from ingested milk, except in prematures or newborns who may show an increased absorption. Case report of kidney function impairment of a baby whose mother had taken Telmisartan in pregnancy. Until more data on this medication is available, safer alternative drugs are preferred, especially in premature babies or during the neonatal period. Should an ARA-II medication (Sartan type) be necessary, the associated risk may be decreased by choosing the one with a favorable pharmacokinetics (shorter half-life elimination time and lower bioavailability) like Eprosartan and Losartan
Losartan Potassium And Hydrochlorothiazide Tablet Breastfeeding Analsys - 2
Hydrochlorothiazide while Breastfeeding
CAS Number: 58-93-5
Hydrochlorothiazide doses of 50 mg daily or less are acceptable during lactation. Intense diuresis with large doses may decrease breastmilk production.
Losartan potassium while Breastfeeding
CAS Number: 114798-26-4
Because no information is available on the use of losartan during breastfeeding, an alternate drug may be preferred, especially while nursing a newborn or preterm infant.
What should I do if already breastfed my kid after using Losartan Potassium And Hydrochlorothiazide Tablet?
During whole lactation period you shall first discuss with your doctor and then together you shall decide whether you shall take that drug or not however if you have already taken Losartan Potassium And Hydrochlorothiazide Tablet then you shall inform your doctor, But you should not be worried too much as Losartan Potassium And Hydrochlorothiazide Tablet comes in category of low risk drug.
My health care provider has asked me to use Losartan Potassium And Hydrochlorothiazide Tablet, what to do?
Losartan Potassium And Hydrochlorothiazide Tablet comes in category of low risk and if your doctor is aware that you are breastfeeding it should be ok to use
If I am using Losartan Potassium And Hydrochlorothiazide Tablet, will my baby need extra monitoring?
Not much
Who can I talk to if I have questions about usage of Losartan Potassium And Hydrochlorothiazide Tablet in breastfeeding?
US
National Womens Health and Breastfeeding Helpline: 800-994-9662 (TDD 888-220-5446) 9 a.m. and 6 p.m. ET, Monday through Friday
UK
National Breastfeeding Helpline: 0300-100-0212 9.30am to 9.30pm, daily
Association of Breastfeeding Mothers: 0300-330-5453
La Leche League: 0345-120-2918
The Breastfeeding Network supporter line in Bengali and Sylheti: 0300-456-2421
National Childbirth Trust (NCT): 0300-330-0700
Australia
National Breastfeeding Helpline: 1800-686-268 24 hours a day, 7 days a week
Canada
Telehealth Ontario for breastfeeding: 1-866-797-0000 24 hours a day, 7 days a week
