Levocetirizine Dihydrochloride 2% / Mupirocin 2% / Triamcinolone Acetonide 0.025% Cream while Breastfeeding
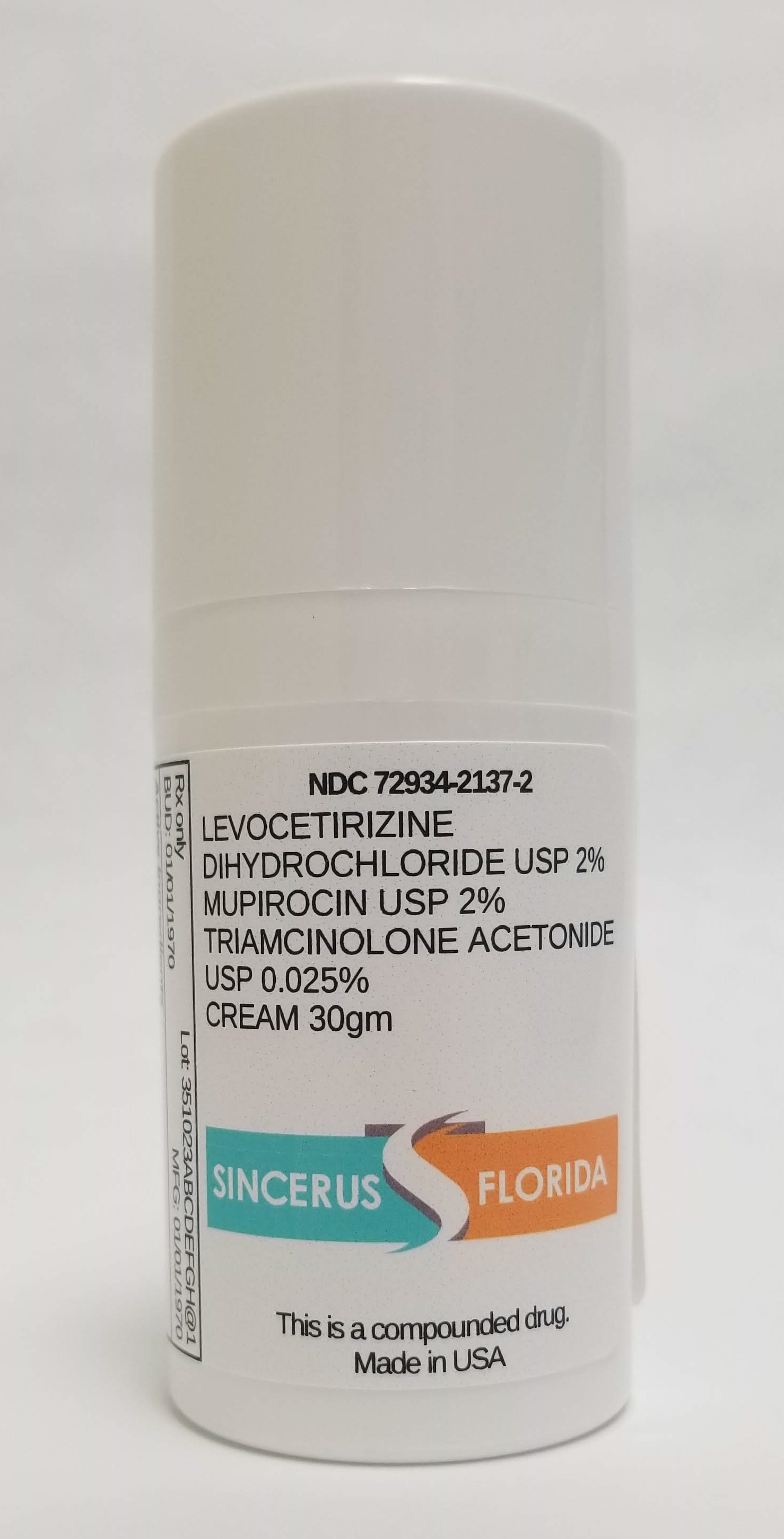
Can I use Levocetirizine Dihydrochloride 2% / Mupirocin 2% / Triamcinolone Acetonide 0.025% Cream while breastfeeding?

Levocetirizine Dihydrochloride 2% / Mupirocin 2% / Triamcinolone Acetonide 0.025% Cream Breastfeeding Analsys
Levocetirizine dihydrochloride while Breastfeeding
Low RiskCAS Number: 130018-77-8
Second generation antihistamine drug derived from piperazine with a minimal sedative effect and low toxicity even at higher dose. On latest update no published data about breastfeeding were found. However, it is the R-enantiomer of cetirizine which is considered to be safe while breastfeeding. No short or long-term side effects were found in an infant with a mother who was treated with Cetirizine in the first month post delivery for pemphigus (Westermann 2012). Because of a high plasma protein binding capacity, excretion into breast milk seems to be unlikely. The British Society of Immunology and Allergy rates Cetirizine as compatible with breastfeeding (Powell 2007).
Mupirocin while Breastfeeding
SafeCAS Number: 12650-69-0
Because of a small dose used and low absorption through skin (less than 1%), excretion into breast milk in significant amount is unlikely. Despite of it is well absorbed by the gut, it is rapidly and completely metabolized into Monic acid which is a non-active metabolite. However, whenever used on the nipple, it is recommended remove excess of cream by using a gauze. Effectiveness is not higher than purified Lanolin for treatment of sore or cracked nipples. Results in the treatment of nipple infection due to Staph. aureus are less encouraging than with the use of oral antibiotics. Caution should be observed with the application of creams, gels and other products that are indicated for local use if they contain paraffin (Mineral oil) to avoid absorption by the infant.
Triamcinolone acetonide while Breastfeeding
Low RiskCAS Number: 76-25-5
A corticosteroid with a mainly glucocorticoid action and anti-inflammatory effects of similar strength to that of prednisolone.Systemic administration (oral, injection), inhaled (bronchial, nasal), intra-articular, intravitreous and topical.Indicated in the treatment of rheumatic diseases and collagen, inflammatory bowel disease, dermatitis, asthma, rhinitis, etc. This comment is about systemic, intra-articular and ophthalmic triamcinolone. Since the last update we have not found published data about its excretion in breast milk. Administration of intra-articular triamcinolone in the wrist (Smuin 2016) or via an epidural in the cervical area (McGuire 2012) caused a temporary decrease in the production of milk lasting between one and four weeks that was resolved in both cases via the continuation and stimulation of breastfeeding. The same has occurred, with a shorter duration, following the intra-articular administration of methylprednisolone (Babwah 2013). Although after the administration of triamcinolone, both intraocular (Shen 2010, Degenring 2004), and epidural (Hooten 2016), elimination half-life is about 22-25 days, plasma levels are indetectable or very low, not clinically significant. The maximum concentration peak after these types of administration occurs at 24 hours (Hooten 2016, Shen 2010, Degenring 2004). There is consensus among experts that, in general, neither systemic corticoids nor inhaled ones present a breastfeeding contraindication (National Asthma Education 2004). The low plasma levels obtained after ophthalmic administration suggest a very low risk during breastfeeding. Corticoids are of commonally used in pediatrics and have no side effects when they are used in isolation or in short-term treatments. Until there is more published data about this drug in relation to breastfeeding, alternatives with a safer known pharmacokinetic profile for breastfeeding may be preferable (greater protein binding, lesser half-life and less oral bioavailability), especially during the neonatal period and in case of prematurity. If used during breastfeeding it is advisable to monitor milk production. See below the information of these related products:
Levocetirizine Dihydrochloride 2% / Mupirocin 2% / Triamcinolone Acetonide 0.025% Cream Breastfeeding Analsys - 2
Levocetirizine dihydrochloride while Breastfeeding
CAS Number: 130018-77-8
Levocetirizine is the -enantiomer of cetirizine. Small occasional doses of levocetirizine are probably acceptable during breastfeeding. Larger doses or more prolonged use may cause drowsiness and other effects in the infant or decrease the milk supply, particularly in combination with a sympathomimetic such as pseudoephedrine or before lactation is well established. The British Society for Allergy and Clinical Immunology recommends cetirizine, the racemic form of the drug, at its lowest dose as a preferred choice if an antihistamine is required during breastfeeding.[1]
Mupirocin while Breastfeeding
CAS Number: 12650-69-0
Because less than 1% is absorbed after topical application, mupirocin is considered a low risk to the nursing infant.[1] Ensure that the infant's skin does not come into direct contact with the areas of skin that have been treated. Only water-miscible cream or gel products should be applied to the breast because ointments may expose the infant to high levels of mineral paraffins via licking.[2] Mupirocin applied topically to the nipples appears to be relatively ineffective as a treatment for sore, cracked nipples.
What if I already have used Levocetirizine Dihydrochloride 2% / Mupirocin 2% / Triamcinolone Acetonide 0.025% Cream?
Levocetirizine Dihydrochloride 2% / Mupirocin 2% / Triamcinolone Acetonide 0.025% Cream is in the category of low risk, if you have already used it then its not a big deal if health and behavior of baby is good. However your health care provider shall be aware of the fact that you have used Levocetirizine Dihydrochloride 2% / Mupirocin 2% / Triamcinolone Acetonide 0.025% Cream so you should inform him based on your convenience.
My doctor has prescribed me Levocetirizine Dihydrochloride 2% / Mupirocin 2% / Triamcinolone Acetonide 0.025% Cream, what should I do?
Though Levocetirizine Dihydrochloride 2% / Mupirocin 2% / Triamcinolone Acetonide 0.025% Cream dose not comes in category of safe drugs rather it comes in category of low risk but if your doctor is aware that you are breastfeeding your baby and has still recommended it then its advantages must be outweighing the risks.
If I am using Levocetirizine Dihydrochloride 2% / Mupirocin 2% / Triamcinolone Acetonide 0.025% Cream, will my baby need extra monitoring?
Not much monitoring required while using Levocetirizine Dihydrochloride 2% / Mupirocin 2% / Triamcinolone Acetonide 0.025% Cream
Who can I talk to if I have questions about usage of Levocetirizine Dihydrochloride 2% / Mupirocin 2% / Triamcinolone Acetonide 0.025% Cream in breastfeeding?
US
National Womens Health and Breastfeeding Helpline: 800-994-9662 (TDD 888-220-5446) 9 a.m. and 6 p.m. ET, Monday through Friday
UK
National Breastfeeding Helpline: 0300-100-0212 9.30am to 9.30pm, daily
Association of Breastfeeding Mothers: 0300-330-5453
La Leche League: 0345-120-2918
The Breastfeeding Network supporter line in Bengali and Sylheti: 0300-456-2421
National Childbirth Trust (NCT): 0300-330-0700
Australia
National Breastfeeding Helpline: 1800-686-268 24 hours a day, 7 days a week
Canada
Telehealth Ontario for breastfeeding: 1-866-797-0000 24 hours a day, 7 days a week
