Metabolic Detox while Breastfeeding
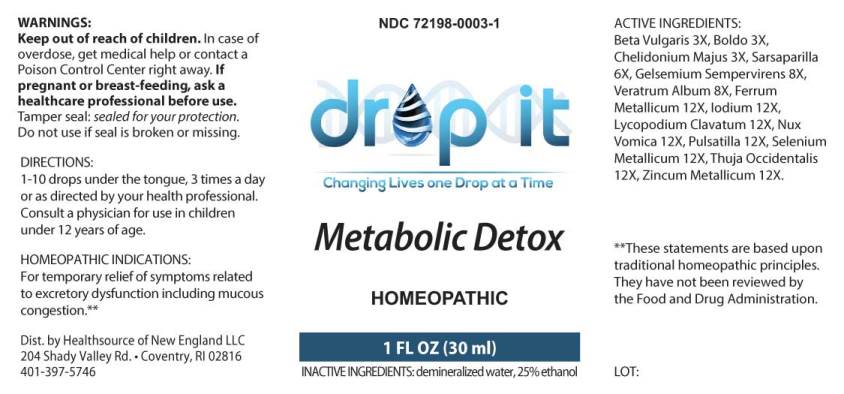
What is Metabolic Detox used for?
Is Metabolic Detox usage safe while breastfeeding? If a lactating mother is using it can there be any effect on growth or development of infant?

Metabolic Detox Breastfeeding Analsys
Sarsaparilla while Breastfeeding
Low RiskCAS Number: 90131-10-5
The roots of this shrub are used. It contains triterpene saponosides, essential oils, starch, choline, mineral salts (K), tannins and phytosterols. Properties traditionally attributed to it without any clinical evidence: diuretic, depurative, sudorific, antirheumatic.Commission E of the German Ministry of Health does not consider any of its indications to be proven and advises against its use (Blumenthal 1998 p.372). Since the last update we have not found published data about its excretion in breast milk. Although apparently lacking toxicity, there are very few publications on this plant and no proven health effects, making its consumption totally non-essential, especially during breastfeeding. Precautions when taking plant preparations: 1. Ensure that they are from a reliable source: poisoning has occurred due to confusing one plant with another with toxic properties, as well as poisoning from heavy metals extracted from the ground and food poisoning due to contamination with bacteria or fungi. 2. Do not take in large amounts; follow recommendations from professional experts in phytotherapy. "Natural" products are not always good in any quantity: plants contain active substances from which much of our traditional pharmacopoeia has been obtained and can result in poisoning or act as endocrine disruptors if taken in excessive amounts or time periods.
Iron while Breastfeeding
SafeSeveral ferrous salts of iron (ascorbate, aspartate, citrate, chloride, fumarate, gluconate, lactate, oxalate, succinate, sulfate, glycine sulfate, etc.) are used in oral administration for treating or preventing iron deficiency anemia.Its molecular weight varies from 170 for the fumarate and succinate, and from 280 for lactate and sulfate to 400 for aspartate and ascorbate. Characteristics of iron metabolism in the body make unlikely that it would be excreted in a significant amount into breast milk.It is a medication used for treatment of Neonatal Anemia in premature babies. Iron is excreted in small amounts in human milk, usually being enough for covering the daily needs of infants due to its high bioavailability. There is no correlation between mother's daily intake of iron and its concentration in breast milk.Iron supplementation to the mother does not increase levels of iron in breast milk or infant plasma significantly. Excessive supplementation can reduce the zinc concentration in milk. WHO List of Essential Medicines 2002: compatible with breastfeeding.
Iodine while Breastfeeding
UnsafeCAS Number: 7553-56-2
Disinfectant that contains high amount (2-7%) of Iodine in solution with alcohol or water (Lugol's solution) Not absorbed through intact skin of adults. However, it may trespass the inflamed skin, wounds, mucosa surfaces like vagina, in which case can reach concentration in grams in the human serum (1 g = 1,000 milligrams = 1,000,000 micrograms). Normal daily allowance is considered to be as high as 100 to 150 micrograms that increases to 200 – 300 micrograms in pregnancy or nursing period. The latter means less than one third of a milligram. Iodine is concentrated into breast milk with a level that could reach 20 times higher than the concentration in the blood. It has been found higher levels of Iodine, altered results of neonatal screening test for thyroid function, and, transient hypothyroidism in infants whose mothers were exposed to Iodine Povidone. Use should be avoid in the Delivery Room, Operating Room (C-section), Neonatal Units, Toddler admision areas and during the breastfeeding period. Sporadic or inadvertent use, specially on normal skin, does not require special test or procedures because it does not pose higher risk to the child.
Lycopodium clavatum spore while Breastfeeding
UnsafeAerial summits and spores of this fern are used. Traditionally use as a diuretic and intestinal spasm relief drug. Also used for abrasions and skin irritation. It may be a cause of asthma and contact dermatitis.
Strychnos nux-vomica seed while Breastfeeding
DangerousCAS Number: 8046-97-7
Dried seed of this plant has been used. It contains brucine and strychnine. It is highly toxic and easily lethal.
Selenium while Breastfeeding
Low RiskCAS Number: 7782-49-2
Essential trace element necessary for the functioning of the glutathione-peroxidase enzyme system that protects cellular structures from oxidative damage. It is obtained from foods such as vegetables, cereals, legumes, garlic, fish, seafood, eggs and meat. The amount of selenium in these sources depends on the concentration of selenium in the soil. The brazil nut (Bertholletia excelsa) is the food with the highest known concentrations of selenium. Selenium deficiency is very rare. With a staple diet it is not necessary to take selenium supplements in the absence of disease or a condition that may warrant it: parenteral nutrition, Crohn's disease, prematurity (MedlinePlus 2017). Taking too much selenium can cause selenosis, a condition that causes dermatological symptoms (alopecia, nail dystrophy), digestive symptoms, neurological symptoms and fatigue (MedlinePlus 2017).Nutritional supplements containing excessive amounts of selenium have resulted in severe poisoning (Aldosary 2012, Senthilkumaran 2012).The potential effects of selenium on cancer prevention, cardiovascular disease, and heavy metal poisoning and toxins are not proven, so supplementation of selenium other than from normal diet is not recommended (MedlinePlus 2017). The daily needs of selenium for breastfeeding mothers are 70-75 micrograms (mcg) daily. In infants it is 2 to 3 mcg/kg (10 mcg/day during the first 4 months) with a maximum of 30 mcg/day (MedlinePlus 2017, Kipp 2015). Selenium is found naturally in milk in its organic form of selenomethionine (Dorea 2002). The amount of selenium in colostrum is 80 mcg per litre and in mature milk 12-20 mcg/L, with no or very weak correlation with plasma selenium levels or daily intake of selenium (Wasowicz 2001, Bianchi 1999, Artaud 1993, Cummings 1992, Levander 1987, Higashi 1983). However, there are authors who find that selenium supplements for breastfeeding mothers increase selenium levels in milk and infants may exceed their daily needs for selenium. (Dorea 2002, Trafikowska 1996). Better plasma levels of selenium have been found in breastfed infants than in formula-fed infants (Strambi 2004, Sorvacheva 1996). There are lower plasma levels of selenium in babies born small for their gestational age (Strambi 2004).
Zinc while Breastfeeding
SafeZinc (Zn) is an essential element for nutrition. It is present in many foods.Recommended daily allowance of Zn is 8 to 15 mg. (Moran Hall 2010). Millions of people worldwide are Zn-deficient.It is used as a treatment for Wilson's disease and Acrodermatitis Enteropathica. Zn is involved in the regulation process of lactation (Lee 2016).Pasteurization of the milk does not affect the concentration of Zn and other trace elements (Mohd Taufek-2016). The average concentration of Zn in breastmilk is 4 to 16 mg / L (Picciano 1976, Hannan 2005, Dórea 2012) which is independent of plasma levels and maternal daily intake (Krebs 1995, Chierici 1999, Hannan 2009).Intestinal absorption of zinc is almost doubled during pregnancy and lactation (Fung 1997).Zinc levels in the infant are dependent on Zinc levels in the breast milk (Dumrongwongsiri 2015)With a varied and balanced diet, an extra intake of minerals is not needed. Excessive intake of Zinc may cause gastrointestinal problems and Pancytopenia (Irving 2003).
Metabolic Detox Breastfeeding Analsys - 2
Iodine while Breastfeeding
CAS Number: 7553-56-2
Iodine is an essential trace nutrient for all infants that a normal component of breastmilk. Infant requirements are estimated to be 15 mcg/kg daily in fullterm infants and 30 mcg/kg daily in premature infants.[1] Systematic reviews and studies on iodine nutrition found that iodine in breastmilk is adequate in iodine-sufficient countries, but in countries with iodine fortification of foods, many mothers did not obtain adequate iodine and that additional supplementation was desirable.[2][3][4][5] In iodine-deficient areas, supplementation of breastfeeding mothers with iodine appears to be more effective than direct supplementation of the infant in reducing infant iodine deficiency.[6] The American Thyroid Association recommends that breastfeeding women should supplement their diet with a daily oral supplement that contains 150 mcg of iodine, but sustained iodine intake while breastfeeding that exceeds 500 to 1100 mcg daily should be avoided.[7] A survey in the United States between 2011 and 2014 found that only 19% of lactating women used a dietary supplement that contained iodine.[8] The use of excessive amounts of iodine in the mother near term and during breastfeeding (e.g., seaweed soup) can increase breastmilk iodine levels and cause transient hypothyroidism in breastfed infants. The absorption of iodine can be marked after application to open wounds or mucous membranes. Exposure of mothers to unnecessary iodine who are or will be breastfeeding should be avoided or minimized to the extent possible by avoiding its use on maternal mucous membranes (e.g., vaginal use, wound therapy), avoiding prolonged contact time, avoiding repeated applications, and applying it to the smallest possible surface areas of the body. It is possible that maternal exposure to iodine near term could interfere with thyroid studies done as a part of newborn screening tests.
Pulsatilla vulgaris while Breastfeeding
Pulsatilla (Anemone pulsatilla and other related species) contains ranunculin, protoanemonin, and anemonin as well as triterpene saponins and flavonoids. The fresh plant is extremely irritating to the skin, gastrointestinal tract and mucous membranes. Allergic reactions have been reported to pulsatilla. Homeopathic preparations of pulsatilla are reportedly used for sore nipples and mastitis,[1] to reduce an overabundant milk supply,[2] or to increase milk supply.[3] Galactogogues should never replace evaluation and counseling on modifiable factors that affect milk production.[4] No scientifically valid clinical trials support either of these uses. Because of a lack of information, other agents may be preferred in nursing mothers. Dietary supplements do not require extensive pre-marketing approval from the U.S. Food and Drug Administration. Manufacturers are responsible to ensure the safety, but do not need to the safety and effectiveness of dietary supplements before they are marketed. Dietary supplements may contain multiple ingredients, and differences are often found between labeled and actual ingredients or their amounts. A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed
Metabolic Detox Breastfeeding Analsys - 3
Gelsemium sempervirens root and Breastfeeding
UnsafeAll parts of the false jasmine usually contain toxic alkaloids. Eating just one flower has reportedly been lethal to children. The plant can also cause skin allergies in some people and it is possible that the plant toxins can be absorbed through the skin, especially if there are cuts. It�s not recommended to use false jasmine while breastfeeding. It is acceptable in homeopathic preparation.
Pulsatilla vulgaris and Breastfeeding
Low RiskNote: Mostly safe in Homeopathic preparations
Thuja occidentalis leafy twig and Breastfeeding
Low RiskThuja is one of the most common remedies used for warts. Topical Usage of Thuja for wart is likely safe while breastfeeding. We do not have sufficient safety usage data for Thuja oral consumption, However its likely unsafe to use thuja orally while breastfeeding.
Warning: Tropical usage in breast area shall be avoided to prevent the Thuja passing orally in Infants.What if I already have used Metabolic Detox?
Due to high dilution of ingredients in homeopathic medicines they do not create much problem for baby. Metabolic Detox is a homeopathic medicine and if your baby does not have any abnormal symptoms then there is nothing to worry about. Be careful with too much usage of ethanol based homeopathic medicines during breastfeeding.
I am nursing mother and my doctor has suggested me to use Metabolic Detox, is it safe?
Homeopathic medicines are usually safe in breastfeeding and if Metabolic Detox has been recommended by doctor then there should be no concern about its usage in breastfeeding.
If I am using Metabolic Detox, will my baby need extra monitoring?
Not exactly.
Who can I talk to if I have questions about usage of Metabolic Detox in breastfeeding?
US
National Womens Health and Breastfeeding Helpline: 800-994-9662 (TDD 888-220-5446) 9 a.m. and 6 p.m. ET, Monday through Friday
UK
National Breastfeeding Helpline: 0300-100-0212 9.30am to 9.30pm, daily
Association of Breastfeeding Mothers: 0300-330-5453
La Leche League: 0345-120-2918
The Breastfeeding Network supporter line in Bengali and Sylheti: 0300-456-2421
National Childbirth Trust (NCT): 0300-330-0700
Australia
National Breastfeeding Helpline: 1800-686-268 24 hours a day, 7 days a week
Canada
Telehealth Ontario for breastfeeding: 1-866-797-0000 24 hours a day, 7 days a week
