Bedwetting while Breastfeeding
What is Bedwetting used for?
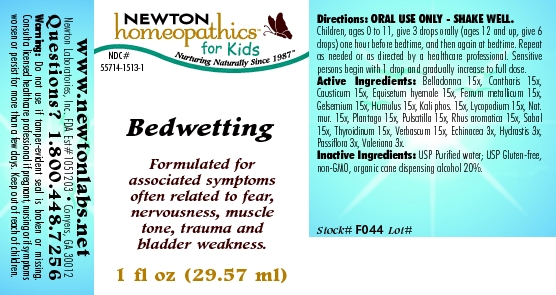
Purpose: OTC - PURPOSE SECTION Formulated for associated symptoms often related to fear, nervousness, muscle tone, trauma and bladder weakness.
Is Bedwetting usage safe while breastfeeding? If a lactating mother is using it can there be any effect on growth or development of infant?

Bedwetting Breastfeeding Analsys
Atropa belladonna while Breastfeeding
UnsafeCAS Number: 8007-93-0
In herbal medicine the leaves of this plant that contains numerous alkaloids are used: l-hyoscyamine and atropine, scopolamine or hyoscine and, all of them potentially high toxic.Traditionally used with poor clinical evidence based on trials as anti-asthmatic, for common colds and intestinal spasms. At latest update no published data on excretion into breast milk were found. With anticholinergic and antimuscarinic properties that may reduce milk production: if necessary take as low dose as possible and avoid long-term treatment if decreasing milk production is observed.Serious side effects (tachycardia, thirst, fever, mydriasis, seizures, coma), especially in infants and newborns (Caksen 2003 Laffargue 2011, Glatstein 2014, Rodríguez-González 2014).There have been cases of gangrene when applied to the chest (Wani 2011). Belladonna may be included in association with other “over the counter" medications of doubtful effectiveness or safety. Overall drug associations are not recommended. Cautions when taking herbal teas:1. Make sure it is obtained from a reliable source: reportedly, poisonings have occurred due to confusion after using another plant with toxic effects (Hsu 1995), some others contain heavy metals that may cause poisoning and others may cause food poisoning due to contamination with bacteria or fungi.2. Do not take it excessively. "Natural" products are not always good in any amount: plants contain active substances from which are made many compounds of our traditional pharmacopoeia that can cause poisoning if consumed in exaggerated quantities or for long periods.
Iron while Breastfeeding
SafeSeveral ferrous salts of iron (ascorbate, aspartate, citrate, chloride, fumarate, gluconate, lactate, oxalate, succinate, sulfate, glycine sulfate, etc.) are used in oral administration for treating or preventing iron deficiency anemia.Its molecular weight varies from 170 for the fumarate and succinate, and from 280 for lactate and sulfate to 400 for aspartate and ascorbate. Characteristics of iron metabolism in the body make unlikely that it would be excreted in a significant amount into breast milk.It is a medication used for treatment of Neonatal Anemia in premature babies. Iron is excreted in small amounts in human milk, usually being enough for covering the daily needs of infants due to its high bioavailability. There is no correlation between mother's daily intake of iron and its concentration in breast milk.Iron supplementation to the mother does not increase levels of iron in breast milk or infant plasma significantly. Excessive supplementation can reduce the zinc concentration in milk. WHO List of Essential Medicines 2002: compatible with breastfeeding.
Hops while Breastfeeding
Low RiskCAS Number: 977070-67-9
Climbing plant. The female inflorescences or flower tips are used.It contains phloroglucinols, estrogenic, quercetin, kaempferol, tannins, phenolic acids essential oil and flavonoids. One of its components, 8-prenylnaringenin (8-PN) is the most powerful phytoestrogen known. Properties that are attributed: hypnotic, sedative, orexigenic.It is used as a flavoring and stabilizer of the beer.Indications German Commission E Ministry of Health, EMA and ESCOP: insomnia, nervousness, anxiety There is no scientific evidence showing an improvement in milk production.A possible estrogenic effect may be a decrease in milk production.The best galactogogue is a frequent and on-demand breastfeeding along with proper technique. During breastfeeding its consumption should be moderate or occasional.
Potassium phosphate, dibasic while Breastfeeding
SafeCAS Number: 7447-40-7
Human milk has a potassium concentration of 13 meq/L, almost a half of rehydration solution content and a quarter of maximal IV recommended dose. Potassium supplementation does not alter milk concentration without increasing mother’s serum concentration, which is strictly limited from 3,5 to 5,5 meq/L.
Lycopodium clavatum spore while Breastfeeding
UnsafeAerial summits and spores of this fern are used. Traditionally use as a diuretic and intestinal spasm relief drug. Also used for abrasions and skin irritation. It may be a cause of asthma and contact dermatitis.
Sodium chloride while Breastfeeding
SafeCAS Number: 7647-14-5
Sodium chloride either as cooking salt, or, as oral rehydration solution, or, as IV fluid, is entirely compatible with BF.
Saw palmetto while Breastfeeding
Low RiskCAS Number: 84604-15-9
The fruits from this palm tree with a high content of fatty acids (oleic, lauric, myristic, linoleic and linolenic acids) are used. They also contain flavonoids and phytosterols (beta-sitosterol) that exert both an antiandrogenic and estrogenic action It is used for treatment of prostate hyperplasia. Also used, however on a poor scientific basis, for treatment of androgenic alopecia and hirsutism (Murugusundram 2009, Rossi 2012, Wessagowit 2016).. It has been related to some problems such as hormonal disruption when it was used in girls (Morabito 2015), but mostly without serious side effects (Agbabiaka 2009). At latest update no published data on excretion into breast milk were found. No likely risk when topically used, whenever it is not applied on the chest.A moderate consumption would not represent a risk while breastfeeding. It may be prudent to avoid using it during the neonatal period (within first month after birth) and in cases of prematurity. Cautions when taking herbal teas:1. Make sure it is obtained from a reliable source: reportedly, poisonings have occurred due to confusion after using another plant with toxic effects, some others contain heavy metals that may cause poisoning and others may cause food poisoning due to contamination with bacteria or fungi.2. Do not take it excessively. "Natural" products are not always good in any amount: plants contain active substances from which are made many compounds of our traditional pharmacopoeia that can cause poisoning if consumed in exaggerated quantities or for long periods.
Echinacea, unspecified while Breastfeeding
Low RiskCAS Number: 84696-11-7
Plant that is widely used even during pregnancy and breastfeeding. Because a lack of toxicity with an appropriate dose and moderate consumption it should be compatible with breastfeeding. The roots and aerial summits are used. It contains polysaccharides, essential oil, flavonoids, pyrrolizidine alkaloids among others. Unproven effects: immune stimulant, wound healing, anti-inflammatory. Indications are: common cold, bronchitis, skin lesions.Roots and aerial summits are used. It contains polysaccharides, essential oil, flavonoids, pyrrolizidine alkaloids ... Unproven effects: immune stimulant, wound healing, anti-inflammatory. Indications according to Commission E of German Ministry of Health: common cold, bronchitis, skin lesions. Contrary to the European Scientific Cooperative on Phytotherapy (ESCOP), the European Medication Agency does not recommend usage in younger than 12 years (allergy risk). Avoid using for longer than 8 weeks (risk for leukopenia)
Passiflora incarnata flowering top while Breastfeeding
Low RiskCAS Number: 8057-62-3
At latest update, relevant information on excretion into breast milk was not found. Aerial summits of this climbing plant are used. Constituents are: flavonoids, pyranics, heterosides, alkaloids. Attributed effects with only weak scientific evidence on effectiveness are: sedative, hypnotic, anti-spasmodic. Because of paucity of data on toxicity, recommendations done are to use it at low doses for short term periods. The European Medicines Agency does not authorize its use for children younger than 12 years old , pregnancy and breastfeeding. When used while breastfeeding, it is recommended to use it at low dose for a short-term period. Following-up the infant for sedation is recommended.
Valerian while Breastfeeding
Low RiskCAS Number: 8057-49-6
At last update significant data on breastfeeding were not found. A commonly used herb in many cultures and countries, even during pregnancy and breastfeeding with very few reported side-effects. Whenever not abused it has a low toxicity. Moderate use is considered to be compatible with breastfeeding, however because of the possibility of sedative effect in infants should better be avoided in cases of prematurity and in the neonatal period. Be aware of sedative effects in the infant. Roots, rhizomes and stolons of the plant are used. It contains iridoids, valepotriates, steroids, essential oils, GABA and tannins. Unproven beneficial effects in adults: sedative, hypnotic, anti-spasmodic. Indication after Commission E of German Ministry of Health: insomnia, nervousness, anxiety. Maximal daily dose: 9 g (2 g of dried extract)
Bedwetting Breastfeeding Analsys - 2
Atropa belladonna while Breastfeeding
CAS Number: 8007-93-0
Belladonna (Atropa belladonna) contains anticholinergic alkaloids such as atropine and scopolamine. Belladonna has been used in the past for headache, airway obstruction, and irritable bowel syndrome among others, but its use has been supplanted by more specific and less toxic compounds. Long-term use of belladonna might reduce milk production by reducing serum prolactin.[1] Application of belladonna paste to the nipple to reduce milk secretion during lactation is an extremely old use.[2] However, it is still used this way in rural India for treating breast abscesses and may have contributed to cases of breast gangrene.[3] Because of the narrow therapeutic index and variable potency of plant-based (i.e., nonstandardized) belladonna, it should be avoided orally and topically during lactation. Homeopathic products are not likely to interfere with breastfeeding or cause toxicity. Dietary supplements do not require extensive pre-marketing approval from the U.S. Food and Drug Administration. Manufacturers are responsible to ensure the safety, but do not need to the safety and effectiveness of dietary supplements before they are marketed. Dietary supplements may contain multiple ingredients, and differences are often found between labeled and actual ingredients or their amounts. A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed information #about dietary supplements# is available elsewhere on the LactMed Web site.
Hops while Breastfeeding
Hops (Humulus lupulus) contains bitter acids, flavonoids, phytoestrogens (e.g., 8-prenylnaringenin), and essential oil. Hops is a purported galactogogue.[1] Some animal evidence indicates that a polysaccharide in hops can increase serum prolactin.[2] However, a small study in humans found that a hops soup appeared to lower serum prolactin levels.[3] Galactogogues should never replace evaluation and counseling on modifiable factors that affect milk production.[4] No data exist on the excretion of any components of hops into breastmilk or on the safety and efficacy of hops in nursing mothers or infants. Hops is "generally recognized as safe" (GRAS) as a food by the U.S. Food and Drug Administration. Hops can cause sedation and should be avoided while taking other sedating drugs and in patients with depression. Allergy to hops occurs rarely. Some sources recommend avoiding hops during breastfeeding because of its phytoestrogen content. Dietary supplements do not require extensive pre-marketing approval from the U.S. Food and Drug Administration. Manufacturers are responsible to ensure the safety, but do not need to the safety and effectiveness of dietary supplements before they are marketed. Dietary supplements may contain multiple ingredients, and differences are often found between labeled and actual ingredients or their amounts. A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed information #about dietary supplements# is available elsewhere on the LactMed Web site.
Pulsatilla vulgaris while Breastfeeding
Pulsatilla (Anemone pulsatilla and other related species) contains ranunculin, protoanemonin, and anemonin as well as triterpene saponins and flavonoids. The fresh plant is extremely irritating to the skin, gastrointestinal tract and mucous membranes. Allergic reactions have been reported to pulsatilla. Homeopathic preparations of pulsatilla are reportedly used for sore nipples and mastitis,[1] to reduce an overabundant milk supply,[2] or to increase milk supply.[3] Galactogogues should never replace evaluation and counseling on modifiable factors that affect milk production.[4] No scientifically valid clinical trials support either of these uses. Because of a lack of information, other agents may be preferred in nursing mothers. Dietary supplements do not require extensive pre-marketing approval from the U.S. Food and Drug Administration. Manufacturers are responsible to ensure the safety, but do not need to the safety and effectiveness of dietary supplements before they are marketed. Dietary supplements may contain multiple ingredients, and differences are often found between labeled and actual ingredients or their amounts. A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed
Thyroid, unspecified while Breastfeeding
CAS Number: 8028-36-2
Thyroid is an animal-derived mixture of levothyroxine (T4) and liothyronine (T3), which are normal components of human milk. Limited data on exogenous replacement doses of levothyroxine during breastfeeding indicate no adverse effects in infants. If thyroid is required by the mother, it is not a reason to discontinue breastfeeding. The American Thyroid Association recommends that subclinical and overt hypothyroidism should be treated with levothyroxine in lactating women seeking to breastfeed.[1] Thyroid dosage requirement may be increased in the postpartum period compared to prepregnancy requirements patients with Hashimoto's thyroiditis.[2]
Echinacea, unspecified while Breastfeeding
CAS Number: 84696-11-7; 90028-20
Echinacea species (Echinacea angustifolia, Echinacea purpurea, Echinacea pallida) contain high molecular weight polysaccharides (e.g., heteroxylan, arabinogalactan) and lower molecular weight compounds (e.g., alkylamides, caffeoyl conjugates such as cichoric acid and echinacosides), but no single chemical is known to be responsible for echinacea's biological activity. Some products have been standardized based on echinacoside, and others on cichoric acid. Echinacea has no specific uses during breastfeeding, but is commonly used orally to treat or prevent upper respiratory infections. It is also used topically to treat skin infections. Excretion of some of the purportedly active alkamides was found in breastmilk in one mother. No data exist on the safety and efficacy of echinacea in nursing mothers or infants. In general, echinacea is well tolerated with gastrointestinal upset, diarrhea and constipation, skin rash and rarely allergic reactions reported. It may also alter the metabolism of some dugs metabolized by the P450 enzyme system. Some sources indicate that echinacea is safe in recommended doses,[1] while others recommend avoiding it during breastfeeding because of the lack of published safety data. Dietary supplements do not require extensive pre-marketing approval from the U.S. Food and Drug Administration. Manufacturers are responsible to ensure the safety, but do not need to the safety and effectiveness of dietary supplements before they are marketed. Dietary supplements may contain multiple ingredients, and differences are often found between labeled and actual ingredients or their amounts. A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed information #about dietary supplements# is available elsewhere on the LactMed Web site.
Goldenseal while Breastfeeding
CAS Number: 84603-60-1
Goldenseal (Hydrastis canadensis) root contains berberine and other isoquinoline alkaloids. Goldenseal has traditionally been used as an anti-infective both systemically and topically, although high-quality studies of its efficacy and safety are lacking. It has also been used to mask illicit drugs in the urine, although it appears to be ineffective with modern laboratory methods. Goldenseal has been used topically by nursing mothers to treat sore nipples.[1] No data exist on the excretion of any components of goldenseal into breastmilk or on the safety and efficacy of goldenseal in nursing mothers. Berberine can displace bilirubin from serum albumin, causing concern about exposure of newborn infants, because bilirubin can build up in the infant's brain, causing brain damage. However, the extent of berberine's passage from the mother to the infant is unknown. Most sources recommend avoiding exposure of neonates to goldenseal via breastfeeding or otherwise.[2][3][4] Dietary supplements do not require extensive pre-marketing approval from the U.S. Food and Drug Administration. Manufacturers are responsible to ensure the safety, but do not need to the safety and effectiveness of dietary supplements before they are marketed. Dietary supplements may contain multiple ingredients, and differences are often found between labeled and actual ingredients or their amounts. A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed information #about dietary supplements# is available elsewhere on the LactMed Web site.
Valerian while Breastfeeding
CAS Number: 8008-88-6; 8057-49-6
Valerian (Valeriana officinalis) root contains mono- and sesquiterpenes, and iridoid triesters (valepotriates). Preparations are sometimes standardized on valerenic acid content. Valerian has no specific uses in nursing mothers, but is most commonly used to treat anxiety and sleep disturbances, and occasionally for self-treatment of postpartum blues or depression.[1][2] No data exist on the safety and efficacy of valerian in nursing mothers or infants. In general, valerian is well tolerated, with side effects such as dizziness, hangover or headache reported occasionally. Valerian is "generally recognized as safe" (GRAS) for use in food by the U.S. Food and Drug Administration. Valerian is often not recommended during lactation because of the theoretical concerns over its valepotriates and baldrinals which have been shown to be cytotoxic and mutagenic in vitro. Because there is no published experience with valerian during breastfeeding, an alternate therapy may be preferred, especially while nursing a newborn or preterm infant. Dietary supplements do not require extensive pre-marketing approval from the U.S. Food and Drug Administration. Manufacturers are responsible to ensure the safety, but do not need to the safety and effectiveness of dietary supplements before they are marketed. Dietary supplements may contain multiple ingredients, and differences are often found between labeled and actual ingredients or their amounts. A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed information #about dietary supplements# is available elsewhere on the LactMed Web site.
Bedwetting Breastfeeding Analsys - 3
Gelsemium sempervirens root and Breastfeeding
UnsafeAll parts of the false jasmine usually contain toxic alkaloids. Eating just one flower has reportedly been lethal to children. The plant can also cause skin allergies in some people and it is possible that the plant toxins can be absorbed through the skin, especially if there are cuts. It�s not recommended to use false jasmine while breastfeeding. It is acceptable in homeopathic preparation.
Pulsatilla vulgaris and Breastfeeding
Low RiskNote: Mostly safe in Homeopathic preparations
Thyroid, unspecified and Breastfeeding
SafeGoldenseal and Breastfeeding
UnsafeWhat if I already have used Bedwetting?
Due to high dilution of ingredients in homeopathic medicines they do not create much problem for baby. Bedwetting is a homeopathic medicine and if your baby does not have any abnormal symptoms then there is nothing to worry about. Be careful with too much usage of ethanol based homeopathic medicines during breastfeeding.
I am nursing mother and my doctor has suggested me to use Bedwetting, is it safe?
Homeopathic medicines are usually safe in breastfeeding and if Bedwetting has been recommended by doctor then there should be no concern about its usage in breastfeeding.
If I am using Bedwetting, will my baby need extra monitoring?
Not exactly.
Who can I talk to if I have questions about usage of Bedwetting in breastfeeding?
US
National Womens Health and Breastfeeding Helpline: 800-994-9662 (TDD 888-220-5446) 9 a.m. and 6 p.m. ET, Monday through Friday
UK
National Breastfeeding Helpline: 0300-100-0212 9.30am to 9.30pm, daily
Association of Breastfeeding Mothers: 0300-330-5453
La Leche League: 0345-120-2918
The Breastfeeding Network supporter line in Bengali and Sylheti: 0300-456-2421
National Childbirth Trust (NCT): 0300-330-0700
Australia
National Breastfeeding Helpline: 1800-686-268 24 hours a day, 7 days a week
Canada
Telehealth Ontario for breastfeeding: 1-866-797-0000 24 hours a day, 7 days a week
