Fever - Infection 56.7 G while Breastfeeding
What is Fever - Infection 56.7 G used for?
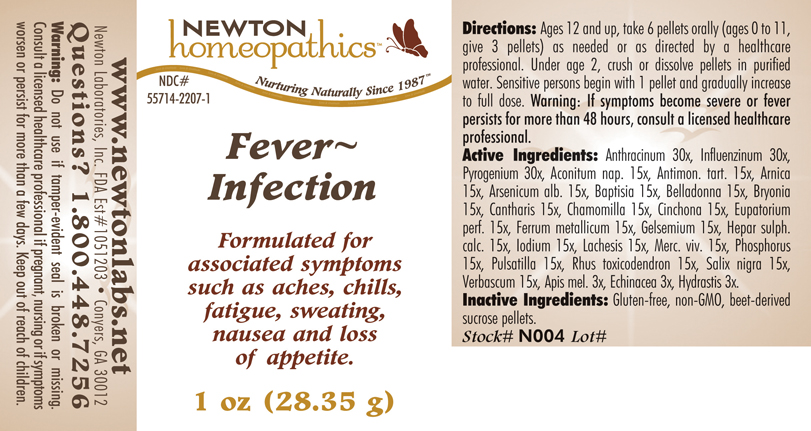
Purpose: OTC - PURPOSE SECTION Formulated for associated symptoms such as aches, chills, fatigue, sweating, nausea and loss of appetite
Is Fever - Infection 56.7 G usage safe while breastfeeding? If a lactating mother is using it can there be any effect on growth or development of infant?

Fever - Infection 56.7 G Breastfeeding Analsys
Influenza a virus while Breastfeeding
SafeVaccines are usually compatible with breastfeeding either if they are formed by live, attenuated, inactivated, death strains or microorganism toxoid. Except for rubella vaccine, they are not excreted into breast milk and do not cause harm to the infant. Yellow fever vaccine has a higher risk for harm effect on infants younger than 6 months old (Consult information on a particular vaccine at our web). Breastfeeding may enhance antibody response to vaccines. Early postpartum period is appropriate to get mothers vaccinated against measles, rubella and mumps in case they were not immunized. Breastfeeding mothers should be protected by providing recommended vaccination for adults.
Aconitum napellus while Breastfeeding
SafeThe flowers and roots and leaves of this herbaceous plant are used. It contains sesquiterpene lactones, essential oil, flavonoids and traces of pyrrolizidine alkaloids. Topical use on whole skin. Indications in traditional medicine without evidence of its effectiveness: topical anti-inflammatory in bruises, sprains and localized muscle pain (EMA 2014). Do not apply to damaged skin It is very toxic orally (Anderson 2017), having described gastroenteritis, cardiac arrhythmia, neurological problems and death (WHO 2007 p.77, nal 2001) in people who took it and a case of severe hemolytic anemia in 9-day-old newborn whose mother was taking arnica infusion (Miller 2009). At the date of the last update, we did not find published data on its excretion in breast milk. The small dose and poor plasma absorption of most topical dermatological preparations make it unlikely that a significant amount will pass into breast milk. Do not apply on the breast so that the infant does not ingest it, or in large areas or for prolonged periods to avoid systemic absorption. Hands should be washed after applying arnica to avoid possible contact with the infants mouth.
Arnica montana while Breastfeeding
SafeCAS Number: 977000-27-3
Se utilizan las flores y también raíces y hojas de esta planta herbácea.Contiene lactonas sesquiterpénicas, aceite esencial, flavonoides y trazas de alcaloides pirrolizidínicos.Uso tópico sobre piel íntegra.Indicaciones en medicina tradicional sin pruebas de su eficacia: antiinflamatorio tópico en contusiones, esguinces y dolores musculares localizados (EMA 2014). No aplicar sobre piel dañada.Es muy tóxica por vía oral (Anderson 2017) habiéndose descrito gastroenteritis, arritmia cardiaca problemas neurológicos y muerte (WHO 2007 p.77, n.a.l. 2001) en personas que la tomaron y un caso de anemia hemolitica grave en un recién nacido de 9 días cuya madre tomaba infusión de arnica (Miller 2009). A fecha de última actualización no encontramos datos publicados sobre su excreción en leche materna. La pequeña dosis y la escasa absorción plasmática de la mayoría de preparaciones dermatológicas tópicas hacen poco probable el paso de cantidad significativa a leche materna. No aplicar sobre el pecho para que el lactante no lo ingiera, ni en áreas extensas o por periodos prolongados para evitar absorción sistémica. Conviene lavarse las manos después de la aplicación de arnica para evitar un posible contacto con la boca del lactante.
Arsenic trioxide while Breastfeeding
DangerousUsed in the treatment of promyelocitic leukemia in adults.
Atropa belladonna while Breastfeeding
UnsafeCAS Number: 8007-93-0
In herbal medicine the leaves of this plant that contains numerous alkaloids are used: l-hyoscyamine and atropine, scopolamine or hyoscine and, all of them potentially high toxic.Traditionally used with poor clinical evidence based on trials as anti-asthmatic, for common colds and intestinal spasms. At latest update no published data on excretion into breast milk were found. With anticholinergic and antimuscarinic properties that may reduce milk production: if necessary take as low dose as possible and avoid long-term treatment if decreasing milk production is observed.Serious side effects (tachycardia, thirst, fever, mydriasis, seizures, coma), especially in infants and newborns (Caksen 2003 Laffargue 2011, Glatstein 2014, Rodríguez-González 2014).There have been cases of gangrene when applied to the chest (Wani 2011). Belladonna may be included in association with other “over the counter" medications of doubtful effectiveness or safety. Overall drug associations are not recommended. Cautions when taking herbal teas:1. Make sure it is obtained from a reliable source: reportedly, poisonings have occurred due to confusion after using another plant with toxic effects (Hsu 1995), some others contain heavy metals that may cause poisoning and others may cause food poisoning due to contamination with bacteria or fungi.2. Do not take it excessively. "Natural" products are not always good in any amount: plants contain active substances from which are made many compounds of our traditional pharmacopoeia that can cause poisoning if consumed in exaggerated quantities or for long periods.
Bryonia alba root while Breastfeeding
Low RiskClimbing plant. The female inflorescences or flower tips are used.It contains phloroglucinols, estrogenic, quercetin, kaempferol, tannins, phenolic acids essential oil and flavonoids. One of its components, 8-prenylnaringenin (8-PN) is the most powerful phytoestrogen known. Properties that are attributed: hypnotic, sedative, orexigenic.It is used as a flavoring and stabilizer of the beer.Indications German Commission E Ministry of Health, EMA and ESCOP: insomnia, nervousness, anxiety There is no scientific evidence showing an improvement in milk production.A possible estrogenic effect may be a decrease in milk production.The best galactogogue is a frequent and on-demand breastfeeding along with proper technique. During breastfeeding its consumption should be moderate or occasional.
Matricaria recutita while Breastfeeding
SafeCAS Number: 520-36-5
It is a widely used plant even in infants. Because of lack of toxicity, a moderate use is considered to be safe. If topically used, do not apply it on the nipple because risk of contact dermatitis has been reported. There are two different species with similar properties: 1) Common or Sweet Chamomile (Matricaria recutita or Chamomilla recutita). 2) Roman, English or Bitter Chamomile (Anthemis nobilis o Chamaemelum nobile). Inflorescence of the herb is used. Contains Essential Oil, Flavonoids, Lactones and Tannins. Unproven properties are: Anti-spasmodic. Digestive, Anti-inflammatory, Sedative.
Cinchona officinalis bark while Breastfeeding
SafeCinchona alkaloid used in the prophylaxis and treatment of malaria (Pérez 2009). Administered orally or intravenously. It is excreted in breast milk in clinically insignificant amounts (Mathew 2004, Phillips 1986, Terwilliger 1934), much lower than the dose used in newborns and infants (Fulton 1992).No problems have been observed in infants whose mothers were taking it (FDA 2008, Terwilliger 1934). Its use is authorized in infants and children.Avoid in cases of glucose-6-phosphate dehydrogenase deficiency (Mathew 2004, WHO/UNICEF 2002, Fulton 1992). American Academy of Pediatrics: medication usually compatible with breastfeeding (AAP 2001). WHO list of essential medicines: compatible with breastfeeding (WHO / UNICEF, 2002).
Iron while Breastfeeding
SafeSeveral ferrous salts of iron (ascorbate, aspartate, citrate, chloride, fumarate, gluconate, lactate, oxalate, succinate, sulfate, glycine sulfate, etc.) are used in oral administration for treating or preventing iron deficiency anemia.Its molecular weight varies from 170 for the fumarate and succinate, and from 280 for lactate and sulfate to 400 for aspartate and ascorbate. Characteristics of iron metabolism in the body make unlikely that it would be excreted in a significant amount into breast milk.It is a medication used for treatment of Neonatal Anemia in premature babies. Iron is excreted in small amounts in human milk, usually being enough for covering the daily needs of infants due to its high bioavailability. There is no correlation between mother's daily intake of iron and its concentration in breast milk.Iron supplementation to the mother does not increase levels of iron in breast milk or infant plasma significantly. Excessive supplementation can reduce the zinc concentration in milk. WHO List of Essential Medicines 2002: compatible with breastfeeding.
Calcium sulfide while Breastfeeding
SafeVarious calcium salts (Acetate, Carbonate, Chloride, Citrate, Phosphate, Gluceptate, Glucobionato, Lactate, Laxctobionato Pidolate, Silicate) are used in the management of hypocalcemia, supplements for treating calcium deficiency states and antacids ( Carbonate and Silicate) Daily requirement of calcium during lactation are 1 g (1.3 g in children under 20 years).Calcium supplements in the diet does not affect the concentration of calcium in milk.Excessive intake of calcium is not good for health. During lactation, consumption of calcium should not exceed 2.5 g a day. WHO List of Essential Medicines 2002 states that it is compatible with breastfeeding.
Iodine while Breastfeeding
UnsafeCAS Number: 7553-56-2
Disinfectant that contains high amount (2-7%) of Iodine in solution with alcohol or water (Lugol's solution) Not absorbed through intact skin of adults. However, it may trespass the inflamed skin, wounds, mucosa surfaces like vagina, in which case can reach concentration in grams in the human serum (1 g = 1,000 milligrams = 1,000,000 micrograms). Normal daily allowance is considered to be as high as 100 to 150 micrograms that increases to 200 – 300 micrograms in pregnancy or nursing period. The latter means less than one third of a milligram. Iodine is concentrated into breast milk with a level that could reach 20 times higher than the concentration in the blood. It has been found higher levels of Iodine, altered results of neonatal screening test for thyroid function, and, transient hypothyroidism in infants whose mothers were exposed to Iodine Povidone. Use should be avoid in the Delivery Room, Operating Room (C-section), Neonatal Units, Toddler admision areas and during the breastfeeding period. Sporadic or inadvertent use, specially on normal skin, does not require special test or procedures because it does not pose higher risk to the child.
Mercury while Breastfeeding
Low RiskCAS Number: 7439-97-6
Environmental pollutant that is used for manufacturation of batteries, fungicidal products, dental amalgam, and contaminated fish. Most of mercury present in breast milk does it as an inorganic substance which is almost non-absorbable. Breastfeeding should be discontinued whenever a mother is contaminated or intoxicated. It may be a source of neurological troubles. Benefits of breastfeeding are largely more important than risk related to the presence of mild level environment pollutants in human milk, in many instances, they are at lower content than those found in cow’s milk or other foods. (Codex alimentarius FAO-WHO).
Echinacea, unspecified while Breastfeeding
Low RiskCAS Number: 84696-11-7
Plant that is widely used even during pregnancy and breastfeeding. Because a lack of toxicity with an appropriate dose and moderate consumption it should be compatible with breastfeeding. The roots and aerial summits are used. It contains polysaccharides, essential oil, flavonoids, pyrrolizidine alkaloids among others. Unproven effects: immune stimulant, wound healing, anti-inflammatory. Indications are: common cold, bronchitis, skin lesions.Roots and aerial summits are used. It contains polysaccharides, essential oil, flavonoids, pyrrolizidine alkaloids ... Unproven effects: immune stimulant, wound healing, anti-inflammatory. Indications according to Commission E of German Ministry of Health: common cold, bronchitis, skin lesions. Contrary to the European Scientific Cooperative on Phytotherapy (ESCOP), the European Medication Agency does not recommend usage in younger than 12 years (allergy risk). Avoid using for longer than 8 weeks (risk for leukopenia)
Influenza b virus while Breastfeeding
SafeVaccines are usually compatible with breastfeeding either if they are formed by live, attenuated, inactivated, death strains or microorganism toxoid. Except for rubella vaccine, they are not excreted into breast milk and do not cause harm to the infant. Yellow fever vaccine has a higher risk for harm effect on infants younger than 6 months old (Consult information on a particular vaccine at our web). Breastfeeding may enhance antibody response to vaccines. Early postpartum period is appropriate to get mothers vaccinated against measles, rubella and mumps in case they were not immunized. Breastfeeding mothers should be protected by providing recommended vaccination for adults.
Fever - Infection 56.7 G Breastfeeding Analsys - 2
Arsenic trioxide while Breastfeeding
CAS Number: 1327-53-3
Most sources consider breastfeeding to be contraindicated during maternal antineoplastic drug therapy. It might be possible to breastfeed safely during intermittent therapy with an appropriate period of breastfeeding abstinence; the manufacturer recommends an abstinence period of 1 week after the last dose. Chemotherapy may adversely affect the normal microbiome and chemical makeup of breastmilk.[1] Women who receive chemotherapy during pregnancy are more likely to have difficulty nursing their infant.[2]
Atropa belladonna while Breastfeeding
CAS Number: 8007-93-0
Belladonna (Atropa belladonna) contains anticholinergic alkaloids such as atropine and scopolamine. Belladonna has been used in the past for headache, airway obstruction, and irritable bowel syndrome among others, but its use has been supplanted by more specific and less toxic compounds. Long-term use of belladonna might reduce milk production by reducing serum prolactin.[1] Application of belladonna paste to the nipple to reduce milk secretion during lactation is an extremely old use.[2] However, it is still used this way in rural India for treating breast abscesses and may have contributed to cases of breast gangrene.[3] Because of the narrow therapeutic index and variable potency of plant-based (i.e., nonstandardized) belladonna, it should be avoided orally and topically during lactation. Homeopathic products are not likely to interfere with breastfeeding or cause toxicity. Dietary supplements do not require extensive pre-marketing approval from the U.S. Food and Drug Administration. Manufacturers are responsible to ensure the safety, but do not need to the safety and effectiveness of dietary supplements before they are marketed. Dietary supplements may contain multiple ingredients, and differences are often found between labeled and actual ingredients or their amounts. A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed information #about dietary supplements# is available elsewhere on the LactMed Web site.
Matricaria recutita while Breastfeeding
CAS Number: 8002-66-2
Two different plant species with similar effects are known as chamomile: German chamomile (Matricaria recutita) and Roman chamomile (Chamaemelum nobile). Both contain similar ingredients, including sesquiterpenes (e.g., bisabolol, farnesene), sesquiterpenelactones (e.g., chamazulene, matricin), flavonoids (e.g., apigenin, luteolin), and volatile oils. Chamomile is used orally as a sedative and for gastrointestinal conditions; it is used topically for wound healing. Both herbal and homeopathic preparations have been used to treat mastitis and cracked, bleeding nipples.[1] Chamomile has been used as a galactogogue;[2][3] however, no scientifically valid clinical trials support this use. Galactogogues should never replace evaluation and counseling on modifiable factors that affect milk production.[4] Chamomile is "generally recognized as safe" (GRAS) for use in food by the U.S. Food and Drug Administration as a spice, seasoning, or flavoring agent. No data exist on the safety of chamomile in nursing mothers or infants, although rare sensitization may occur (see below).[5] It has been safely and effectively used alone and with other herbs in infants for the treatment of colic, diarrhea, and other conditions,[6][7][8][9] so the smaller amounts expected (but not demonstrated) in breastmilk are likely not to be harmful with usual maternal doses. Note Clostridium botulinum (botulism) spores have been found in some loose-leaf chamomile teas sold in health food stores. Topical chamomile is a known sensitizing agent, even with homeopathic products.[10] Two women developed contact dermatitis of the nipples and areolas after applying Kamillosan ointment for cracked nipples. The product was purchased in England and contained 10.5% Roman chamomile extracts and oil. Reactions were confirmed to be caused by Roman chamomile by patch testing in both women. Drinking chamomile tea can exacerbate topical skin rashes and has caused anaphylaxis in sensitized individuals.[11] Chamomile has possible cross-reactivity with other members of the aster family (e.g., echinacea, feverfew, and milk thistle).[5] Dietary supplements do not require extensive pre-marketing approval from the U.S. Food and Drug Administration. Manufacturers are responsible to ensure the safety, but do not need to the safety and effectiveness of dietary supplements before they are marketed. Dietary supplements may contain multiple ingredients, and differences are often found between labeled and actual ingredients or their amounts. A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed information #about dietary supplements# is available elsewhere on the LactMed Web site.
Cinchona officinalis bark while Breastfeeding
CAS Number: 130-95-0
Because of the low levels of quinine in breastmilk, amounts ingested by the infant are small and would not be expected to cause any adverse effects in breastfed infants. The dosage in milk is far below those required to treat an infant for malaria.[1] However, quinine should not be used in mothers with an infant who is glucose-6-phosphate dehydrogenase (G6PD) deficient.[2] Even the relatively small amounts of quinine in tonic water ingested by the mother have caused hemolysis in G6PD-deficient infants.
Iodine while Breastfeeding
CAS Number: 7553-56-2
Iodine is an essential trace nutrient for all infants that a normal component of breastmilk. Infant requirements are estimated to be 15 mcg/kg daily in fullterm infants and 30 mcg/kg daily in premature infants.[1] Systematic reviews and studies on iodine nutrition found that iodine in breastmilk is adequate in iodine-sufficient countries, but in countries with iodine fortification of foods, many mothers did not obtain adequate iodine and that additional supplementation was desirable.[2][3][4][5] In iodine-deficient areas, supplementation of breastfeeding mothers with iodine appears to be more effective than direct supplementation of the infant in reducing infant iodine deficiency.[6] The American Thyroid Association recommends that breastfeeding women should supplement their diet with a daily oral supplement that contains 150 mcg of iodine, but sustained iodine intake while breastfeeding that exceeds 500 to 1100 mcg daily should be avoided.[7] A survey in the United States between 2011 and 2014 found that only 19% of lactating women used a dietary supplement that contained iodine.[8] The use of excessive amounts of iodine in the mother near term and during breastfeeding (e.g., seaweed soup) can increase breastmilk iodine levels and cause transient hypothyroidism in breastfed infants. The absorption of iodine can be marked after application to open wounds or mucous membranes. Exposure of mothers to unnecessary iodine who are or will be breastfeeding should be avoided or minimized to the extent possible by avoiding its use on maternal mucous membranes (e.g., vaginal use, wound therapy), avoiding prolonged contact time, avoiding repeated applications, and applying it to the smallest possible surface areas of the body. It is possible that maternal exposure to iodine near term could interfere with thyroid studies done as a part of newborn screening tests.
Pulsatilla vulgaris while Breastfeeding
Pulsatilla (Anemone pulsatilla and other related species) contains ranunculin, protoanemonin, and anemonin as well as triterpene saponins and flavonoids. The fresh plant is extremely irritating to the skin, gastrointestinal tract and mucous membranes. Allergic reactions have been reported to pulsatilla. Homeopathic preparations of pulsatilla are reportedly used for sore nipples and mastitis,[1] to reduce an overabundant milk supply,[2] or to increase milk supply.[3] Galactogogues should never replace evaluation and counseling on modifiable factors that affect milk production.[4] No scientifically valid clinical trials support either of these uses. Because of a lack of information, other agents may be preferred in nursing mothers. Dietary supplements do not require extensive pre-marketing approval from the U.S. Food and Drug Administration. Manufacturers are responsible to ensure the safety, but do not need to the safety and effectiveness of dietary supplements before they are marketed. Dietary supplements may contain multiple ingredients, and differences are often found between labeled and actual ingredients or their amounts. A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed
Echinacea, unspecified while Breastfeeding
CAS Number: 84696-11-7; 90028-20
Echinacea species (Echinacea angustifolia, Echinacea purpurea, Echinacea pallida) contain high molecular weight polysaccharides (e.g., heteroxylan, arabinogalactan) and lower molecular weight compounds (e.g., alkylamides, caffeoyl conjugates such as cichoric acid and echinacosides), but no single chemical is known to be responsible for echinacea's biological activity. Some products have been standardized based on echinacoside, and others on cichoric acid. Echinacea has no specific uses during breastfeeding, but is commonly used orally to treat or prevent upper respiratory infections. It is also used topically to treat skin infections. Excretion of some of the purportedly active alkamides was found in breastmilk in one mother. No data exist on the safety and efficacy of echinacea in nursing mothers or infants. In general, echinacea is well tolerated with gastrointestinal upset, diarrhea and constipation, skin rash and rarely allergic reactions reported. It may also alter the metabolism of some dugs metabolized by the P450 enzyme system. Some sources indicate that echinacea is safe in recommended doses,[1] while others recommend avoiding it during breastfeeding because of the lack of published safety data. Dietary supplements do not require extensive pre-marketing approval from the U.S. Food and Drug Administration. Manufacturers are responsible to ensure the safety, but do not need to the safety and effectiveness of dietary supplements before they are marketed. Dietary supplements may contain multiple ingredients, and differences are often found between labeled and actual ingredients or their amounts. A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed information #about dietary supplements# is available elsewhere on the LactMed Web site.
Goldenseal while Breastfeeding
CAS Number: 84603-60-1
Goldenseal (Hydrastis canadensis) root contains berberine and other isoquinoline alkaloids. Goldenseal has traditionally been used as an anti-infective both systemically and topically, although high-quality studies of its efficacy and safety are lacking. It has also been used to mask illicit drugs in the urine, although it appears to be ineffective with modern laboratory methods. Goldenseal has been used topically by nursing mothers to treat sore nipples.[1] No data exist on the excretion of any components of goldenseal into breastmilk or on the safety and efficacy of goldenseal in nursing mothers. Berberine can displace bilirubin from serum albumin, causing concern about exposure of newborn infants, because bilirubin can build up in the infant's brain, causing brain damage. However, the extent of berberine's passage from the mother to the infant is unknown. Most sources recommend avoiding exposure of neonates to goldenseal via breastfeeding or otherwise.[2][3][4] Dietary supplements do not require extensive pre-marketing approval from the U.S. Food and Drug Administration. Manufacturers are responsible to ensure the safety, but do not need to the safety and effectiveness of dietary supplements before they are marketed. Dietary supplements may contain multiple ingredients, and differences are often found between labeled and actual ingredients or their amounts. A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed information #about dietary supplements# is available elsewhere on the LactMed Web site.
Fever - Infection 56.7 G Breastfeeding Analsys - 3
Baptisia tinctoria and Breastfeeding
UnsafeWild indigo is an herb. The root is used to make medicine.Wild indigo is used for infections such as diphtheria, influenza (flu), swine flu, the common cold and other upper respiratory tract infections, lymph node infections, scarlet fever, malaria, and typhoid. It is also used for sore tonsils (tonsillitis), sore throat, swelling of the mouth and throat, fever, boils, and Crohns disease. Some people apply wild indigo directly to the skin for ulcers, sore and painful nipples, as a douche for vaginal discharge, and for cleaning open and swollen wounds. Wild indigo is UNSAFE when taken by mouth or applied to the skin, long-term or in large doses. Large doses can cause vomiting, diarrhea, other intestinal problems, and spasms.
While breastfeeding wild indigo is likely not safe when taken by mouth or applied to the skin. Avoid use.
Gelsemium sempervirens root and Breastfeeding
UnsafeAll parts of the false jasmine usually contain toxic alkaloids. Eating just one flower has reportedly been lethal to children. The plant can also cause skin allergies in some people and it is possible that the plant toxins can be absorbed through the skin, especially if there are cuts. It�s not recommended to use false jasmine while breastfeeding. It is acceptable in homeopathic preparation.
Phosphorus and Breastfeeding
SafeNext to calcium, phosphorus is the most abundant mineral in the body, making up about 1% of total body weight. Calcium, which gives strength to bones and teeth, needs to be combined with another mineral, such as phosphorous, to become stabilized before it can be effective.
Phosphorus also helps to release energy from food as it plays an important role in the metabolism of carbohydrate, fat and protein. Phosphorus is naturally found in many food sources and phosphorus supplementation while breastfeeding is mostly safe.
You can easily get all the phosphorus you need from a well-balanced diet (even though most prenatal vitamins dont contain phosphorus). For example, 2 cup of yogurt provides nearly all your phosphorus for the day.
Warning: Consuming high doses of phosphorus for a short time can cause diarrhea or stomach pain. The long term over-consumption of foods high in phosphorus can deplete calcium resources and lead to reduced bone mass, which means that bones are more likely to fracture.Pulsatilla vulgaris and Breastfeeding
Low RiskNote: Mostly safe in Homeopathic preparations
Toxicodendron pubescens leaf and Breastfeeding
SafePoison ivy rash is caused by contact with poison ivy, a plant that grows almost everywhere in the United States. The sap of the poison ivy plant, also known as Toxicodendron radicans, contains oil called urushiol. This is the irritant that causes an allergic reaction and rash.
You dont even have to come in direct contact with the plant to have a reaction. The oil can linger on your gardening equipment, golf clubs, or even your shoes. Brushing against the plant � or anything thats touched it � can result in skin irritation, pain, and itching.
Poison ivy is not contagious. It cannot spread from person to person. It can, however, be spread in a few other scenarios. For example, a pet that encounters poison ivy leaves can carry the urushiol oil in its fur. When you touch the animal, you may pick up the oil and develop a rash. Clothing fibers can also spread poison ivys oil. If you touch poison ivy with a pair of pants or shirt and do not wash it after contact is made, you could develop another rash if you touch the clothing. You can also spread the oil to another person, if they come into contact with clothes that have touched poison ivy. A poison ivy rash cannot spread across your body either. If you come into contact with poison ivy that is burning, you may inhale plant compounds. This can lead to irritation in the lungs, airways, and eyes.
Poison ivy rash doesnt pose a serious risk to a pregnant woman or a developing baby. Your baby can get the rash only from touching something with the oil on it. And the liquid in the blisters doesnt contain urushiol, so the rash cant be spread by scratching or popping them. If you notice a new patch of rash on your baby a few days after the first one appears, its not because the rash has spread. If you have poison ivy it should not affect the milk and health of breastfed baby.
Homeopathic preparations of Poison ivy are used to treat pain, rheumatoid arthritis, menstrual period problems, swelling, and itchy skin disorders. Due to extreme dilution of poison ivy in homeopathic medicines its mostly safe in breastfeeding.
Goldenseal and Breastfeeding
UnsafeWhat should I do if I am breastfeeding mother and I am already exposed to Fever - Infection 56.7 G?
Due to high dilution of ingredients in homeopathic medicines they do not create much problem for baby. Fever - Infection 56.7 G is a homeopathic medicine and if your baby does not have any abnormal symptoms then there is nothing to worry about. Be careful with too much usage of ethanol based homeopathic medicines during breastfeeding.
I am nursing mother and my doctor has suggested me to use Fever - Infection 56.7 G, is it safe?
Homeopathic medicines are usually safe in breastfeeding and if Fever - Infection 56.7 G has been recommended by doctor then there should be no concern about its usage in breastfeeding.
If I am using Fever - Infection 56.7 G, will my baby need extra monitoring?
Not exactly.
Who can I talk to if I have questions about usage of Fever - Infection 56.7 G in breastfeeding?
US
National Womens Health and Breastfeeding Helpline: 800-994-9662 (TDD 888-220-5446) 9 a.m. and 6 p.m. ET, Monday through Friday
UK
National Breastfeeding Helpline: 0300-100-0212 9.30am to 9.30pm, daily
Association of Breastfeeding Mothers: 0300-330-5453
La Leche League: 0345-120-2918
The Breastfeeding Network supporter line in Bengali and Sylheti: 0300-456-2421
National Childbirth Trust (NCT): 0300-330-0700
Australia
National Breastfeeding Helpline: 1800-686-268 24 hours a day, 7 days a week
Canada
Telehealth Ontario for breastfeeding: 1-866-797-0000 24 hours a day, 7 days a week
